“Proprioceptive feedback from extensor muscles during the stance phase ensures that the leg does not go into swing when loaded and that the magnitude of extensor activity is adequate for support. Proprioceptive feedback from flexor muscles towards the end of the stance phase facilitates the initiation of the swing phase of walking. Evidence that muscle afferent feedback also contributes to the magnitude and duration of flexor activity during the swing phase has been demonstrated recently. The regulation of the magnitude and duration of extensor and flexor activity during locomotion is mediated by monosynaptic, disynaptic, and polysynaptic muscle afferent pathways in the spinal cord. In addition to allowing for rapid adaptation in motor output during walking, afferent feedback from muscle proprioceptors is also involved in longer-term adaptations in response to changes in the biomechanical or neuromuscular properties of the walking system.” (2)
Proprioception trumps Biomechanics
As I sit here on a rare Friday afternoon, not working (OK, I am writing this, so sort of working) and looking out at the lake (picture above), while on a family camping trip, I think about a walk on the rocks this morning with my kids. I was watching my very skilled 7 year old jump from rock to rock while my 3 ½ year old, that thinks he is seven, tried to follow his older brother.
I had my foot on a rock which lowered the front of my foot in plantar flexion and stood on that leg. I noticed that my balance was not as great as it was when my foot was in dorsiflexion. This made me think about pronation and supination. Yes, it is not uncommon for me to think about such things, especially when I have some spare time. That is one of the things about being a foot and gait nerd; these sorts of things are always on our minds.
So, why was my balance off? Did I need more proprioceptive work? Were my foot intrinsics having issues? No, it was something much more mundane.
Pronation consists of dorsiflexion, eversion and abduction. This places the foot in a “mobile adaptor” posture, reminiscent of our hunter/gatherer ancestors, who needed to adapt to uneven surfaces while walking over terra firma barefoot. Supination, on the other hand (which is the position my foot was in), consists of plantarflexion, inversion and adduction. It places the foot (particularly the midtarsals) in a locked position for propulsion (think of the foot position during toe off).
So why when my foot was plantar flexed and adducted while standing on this rock so much more unstable in this supposedly more stable, supinated position? I would encourage you, at this point, to try this so you can see what I mean. When I placed my foot in dorsiflexion on the rock, I was much more stable. A most interesting conundrum for a biomechanist.
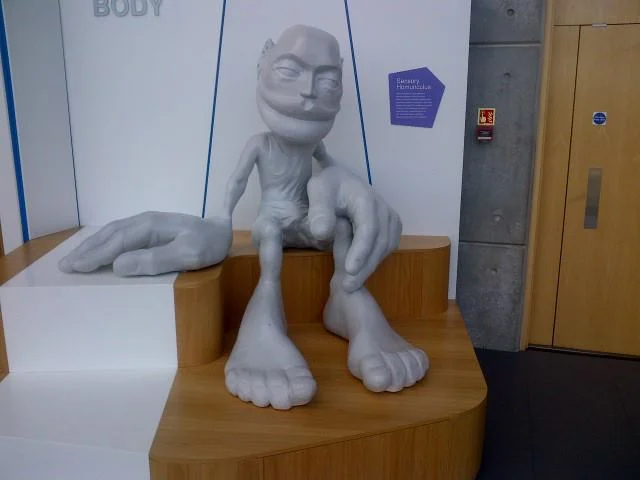
Experimenting for a few minutes, alternating plantar flexion and dorsi flexion, gave me the answer. When we are walking on the flats, our foot is (usually) not pushed to the extremes of dorsiflexion; with the front of the foot up on a rock, it is much more so. This “extra” upward force on the front of the foot, provides much more sensory input (and thus proprioception) from the ball of the feet. Take a look at the sensory homunculus and you can see how much brain real estate is dedicated to your foot, especially the front portion. With this information, we are able to apply more force through the posterior compartment of the leg,which is stronger than my anterior compartment (as it is with most folks).
When the front of your foot is in plantar flexion (ie, your heel is on the rock), we have less sensory input to the balls of the feet, and rely more on the anterior compartment (weaker in many folks, including myself) to counterbalance the weight of our body.
Mystery solved: proprioception trumps biomechanics; more proof that the brain is smarter than we are.
The Gait Guys. Solving the worlds great gait questions, one at a time.
Did you see this in our recent blog post here ? a reader made us look closer. Did you catch it ?
The clients right foot appears to have a dropped 1st met head. (we hate this term, because it is not accurate and is a sloppy clinical description). In this still photo it appears plantarflexed. But in this video, consider the descended 1st met head as due to the disuse or weakness of the EHL muscle (extensor hallucis longus) of the 1st toe. Or, is this in fact a compensated forefoot varus ? Sure looks like it. But with all that anterior compartment weakness (as we discussed in the previous blog post link above) it could just be a mirage. In the photo above, in a normal foot the rearfoot plane (greenline) should parallel the forefoot line (orange line). In this case, in this actively postured foot (thus some inaccuracy here, we are merely making a teaching point from the photo) the upslope of the orange line suggests a forefoot varus. This would be true if the first Metatarsal head also was on this line, but you can see that it has its own idea. This represents, in theory (regarding this photo), a compensated forefoot varus. But remember, this client is holding the foot actively in this posture. A true hands on assessment is needed to truly define a Forefoot varus, and whether it is anatomic, flexible, rigid or in many cases, just a learned functional posturing from weakness of the flexor/extensor pairing of the 1st metatarsal complex or from other weaknesses of the other forefoot evertors. It gets complicated as you can see.
As always, knowledge of the anatomy and functional anatomy allows for observation, and observation leads to understanding, which leads to answers and then remedy implementation. Our thoughts, knowing the case, is that this is a functional appearance illusion of a compensated forefoot varus due to the EHL, EDL and tibialis anterior weakness (anterior compartment) and how they play together with the flexors. One must be sure to assess the EHL when examining the foot. Test all of the muscles one by one. We have been talking about toe extensors for a long time, they can be a paramount steering wheel for the forefoot and arch posture. Podcast 71 talks about this Forefoot varus, and you should care.
In a 2009 study by Reynard et al they concluded:
- “The activity of extensor digitorum longus muscle during the swing phase of gait is important to balance the foot in the frontal plane. The activation of that muscle should be included in rehabilitation programs.” (1)
Have a burning desire to learn more about forefoot varus, here are 25 blog post links from our last few years. And/or you can take our National Shoe Fit program (downloadable links below).
Knowing what you are seeing during your exam and gait analysis can only truly come from coupling your observations with a clinical exam. Anything less is speculation and guess work. It is gambling, and this is not Vegas baby, this is someone’s health.
Shawn and Ivo, The Gait Guys
________________
National Shoe Fit Certification Program:
Gait Guys online /download store (National Shoe Fit Certification and more !) :
http://store.payloadz.com/results/results.aspx?m=80204
1. Foot (Edinb). 2009 Jun;19(2):69-74. Epub 2008 Dec 31. Foot varus in stroke patients: muscular activity of extensor digitorum longus during the swing phase of gait. Reynard F, Dériaz O, Bergeau J.
Other web based Gait Guys lectures:
www.onlinece.com type in Dr. Waerlop or Dr. Allen, ”Biomechanics”Reference
Podcast 71: Forefoot Varus, Big Toe Problems & Charlie Horses"
/*Show sponsor: www.newbalancechicago.com
Lems Shoes. www.lemsshoes.comMention GAIT15 at check out for a 15% discount through August 31st, 2014.
A. Link to our server:
Direct Download:
http://traffic.libsyn.com/thegaitguys/pod_72final.mp3
Permalink: http://thegaitguys.libsyn.com/podcast-71
B. iTunes link:
https://itunes.apple.com/us/podcast/the-gait-guys-podcast/id559864138
C. Gait Guys online /download store (National Shoe Fit Certification and more !) :
http://store.payloadz.com/results/results.aspx?m=80204
D. other web based Gait Guys lectures:
www.onlinece.com type in Dr. Waerlop or Dr. Allen, ”Biomechanics”
______________
Today’s Show notes:
1. American College of Cardiology. Running out your healthy heart. How much exercise is too much ?
http://wgntv.com/2014/07/29/running-for-7-minutes-a-day-cuts-risk-of-death-by-30-study-says/
I’ve been getting bruises that appear on my shin during running. They don’t hurt, I’m just wary of ignoring what could be a warning sign. Have you ever come across this before? (It’s mainly the spot where I had a tibial stress fracture last year, but I also get a few other apparently spontaneous bruises on my lower legs.)
Subtle clues. Helping someone around their anatomy
This patient comes in with low back pain of years duration, helped temporarily with manipulation and activity. Her exam is relatively benign, save for increased lumbar discomfort with axial compression in extension and extension combined with lateral bending. Believe it or not, her abdominal and gluteal muscles (yes, all of them) test strong (no, we couldn’t believe it either; she is extremely regular with her exercises). She has bilateral internal tibial torsion (ITT) and bilateral femoral retro torsion (FRT). She has a decreased progression angle of the feet during walking and the knees do not progress past midlilne. There is a loss of active ankle rocker with gait, but not on the exam table; same with hip extension.
We know she has a sweater on which obscures things a bit, but this is what you have to work with. Look carefully at her posture from the side. The gravitational line should pass from the earlobe, through the shoulder, greater trochanter and through or just anterior to the lateral malleolus.
In the top picture, can you see how her pelvis is anterior to this line? Do you see how it gets worse when she lifts her hands over her head (yes, they are directly over head)? This can signify many things, but often indicates a lack of flexibility in the lumbar lordosis; in this case, she cannot extend her lumbar spine further so she translates her pelvis forward. Most folks should have enough range of motion from a neutral pelvis and enough stability to allow the movement to occur without a significant change. Go ahead, we know you are curious, go watch yourself do this in a mirror and see if YOU change.
Looking at the bottom left picture, can you pick out that she has a genu valgus? Look at the hips and look at the tibial angle.
In the bottom left picture, did you note the progression angle (or lack of) in her feet? This is a common finding (but NOT pathognomonic) in patients with internal tibial torsion. Notice the forefoot adductus on the right foot?
So what do we think is going on?
- ITT and FRT both limit the amount of internal rotation of the thigh and lower leg. Remember you NEED 4 degrees of each to walk normally. Most folks have significantly more
- if you don’t have enough internal rotation of the lower extremity, you will need to “create” it. You can do this by extending the lumbar spine (bottom picture, right) or externally rotating the lower extremity
- Since her ITT and FRT are bilateral, she flexes the pelvis and nutates the pelvis anteriorly.
- the lumbar facet joints should only carry 20% of load
- she is increasing the load and causing facet imbercation resulting in LBP.
What did we do?
- taught her about neutral pelvic positioning, creating more ROM in the lumbar spine
- had her consciously alter her progression angle of her foot on strike, to create more available ROM in internal rotation
- encouraged her to wear neutral shoes
- worked on helping her to create more ankle rocker and hip extension with active drills and exercise (ie gait rehabilitation); shuffle walks, Texas walk, toes up walking, etc
why didn’t we put her in an orthotic to externally rotate her lower extremity? Because with internal tibial torsion, this would move her knee outside the saggital plane and create a biomechanical conflict at the knee and possibly compromising her meniscus.
Cool case, eh? We thought so. Keep on learning so your brain keeps expanding. If you are not growing your brain, you are shrinking it!
The Gait Guys
Here is a great case from a reader.
“Hey guys, I absolutely love the show, especially as it becomes less and less over my head.
Due to your love of gait-altering absurdly thick EVA midsoles, I thought you might like to check out this Hoka incident that occurred at the Marathon des Sable across the Sahara in Morocco, a 6 day 251km event. It was posted by Ian Corless at Talk Ultra Podcast. Apparently the medial side of the midsole collapsed–on DAY 2! This guy finished the race, and as you have to carry 100% of your gear and nutrition, I guess he only had the one pair. It looks like this runner should fly out to CO or IL asap, because if he didn’t have gait issues before, he is sure to have them now.”
This brings up some scary thoughts when it comes to the amount of EVA foam and quality of foam (EVA or otherwise) being used in some shoes. "The more foam there exists, the greater one can break down into their compensation or deforming strategy.“ What do we mean by this ? Well, two things should be on one’s mind: 1. all foam breaks down into the vector of the deforming forces and 2. most of us do not have perfectly clean biomechanics, thus an abnormal loading vector is most likely present. These aberrant biomechanics are eventually reflected into our shoes as a "wear pattern”. In this case, the EVA foam had progressively broken down into their rearfoot pronation (and likely mid and forefoot pronation). In this case, even if the person had enough tibialis posterior and other medial pronation-decelerating structure strength at the start, the acceleration of their foot into this issue is now even more abrupt, brisk, excessive etc. A new pair of shoes would not be broken down into this deformity and so a newer pair of shoes is preventive. This is why we recommend new shoes often, and the cycling in of another pair (or several pair) into the mix so that one is never driving the same shoes into the potentially destructive compensation patterns that most of us have. At least with a fresh pair of shoes brought into the mix at the 200 mile wear point, you would only be in the more destructive shoes every other run, giving the body time to recuperate more.
As for this pair of shoes, this runner either has a terrible right foot problem or this was a brutally flawed right shoe from the get go, or both. We can only imaging how painful the medial knee might be at this point. Furthermore, imagine the abrupt nature of the hip internal rotation mechanics ! IF they do not have hip labrum impingement yet, they will soon ! And with that amount of internal limb spin, can you imagine how inhibited the glutes would be from constantly having to eccentrically control that excessive rotation?
As a whole, are not huge fans of the HOKA shoe family, we just cannot fathom the need for this much foam under the feet. If you have been with us long enough you will have heard on our podcast and blog talk about increased impact forces with increasing EVA foam thickness (want that info, here is the link and references). Just because some EVA foam is good, doesn’t mean more is better. Remember, to propulse off of a foam infrastructure you must bottom out/compress the foam sufficiently to find a firmness to propulse from. The Hoka’s have plenty of foam making this our concern, and we are not picking on just them. There are other companies doing this “super sizing/super stacking” such as Brooks, Altra, and New Balance to name just a few. Sure they have added a greater forefoot rocker/toe spring on the front of the shoe to help (they have to because the foam thickness is so great that there is no flexing of the forefoot of the shoes), but is it enough for you? Remember, every biomechanical phase of the gait cycle is necessary and timely to engage the natural joint, ligament, muscle components of joint loading, mobility, stability and movement. If you spend too much time in one phase (perhaps because you are waiting for foam to decompress) you may wait a moment too long and miss the opportunity for another critical phase to begin in the sequence. This is the root cause of many injuries, aberrant biomechanics leading to aberrant mobility or stability.
So remember these few things:
1. more is not always better for you, it may be for some, but maybe not you.
2. there is a price to pay somewhere in the mechanical system, after all the body is a contained system. What doesn’t happen at one joint often has to be made up at the next proximal or distal joint.
3. Everyone has some aberrant mechanics. No one is perfect. These imperfections will reflect in your shoes, and the longer you are in a pair of shoes the deeper the aberrant mechanics will be reflected in your shoe, thus acting as a steering wheel for the aberrant pattern (the steering is more direct/ more aggressive than in a new pair of shoes). So keep at least 2 pair of shoes rotating in your run cycle, one newer and one half done. We even recommend 3 pairs often. Trust us, the sudden biomechanical shift from a dead shoe into a new one (even though it is a clean new shoe without bad patterns in it) is still a biomechanical shift and could cause adaptive phase problems, pain or injury.
Lots to consider in this game. It is not just about dropping into barefoot and taking off down your street. Not if you want to be doing this for a long time and stay healthy.
Shawn and Ivo, the gait guys
* next day follow up from our social media pages:
Along the lines of EVA and yesterdays post:
“Wear of the EVA consistently increased heel pad stresses, and reduced EVA thickness was the most influential factor, e.g., for a 50% reduction in thickness, peak heel pad stress increased by 19%. ”
This study looks at a model; it would be interesting to see this study with a large cohort.
Role of EVA viscoelastic properties in the protective performance of a sport shoe: computational studies.
ETT and Hip Extension
Not Extra Terrestrial Tricks, but rather External Tibial Torsion. How it effects hip extension.
We received this question from Matthew P on our Facebook post from 8/1 (original post from here) which was based on this article, and thought it would make an excellent opportunity to teach.
“I looked at this yesterday and had actually first come across it a year or more ago when I was trying to find some resources for femoral torsion. You guys are about the only ones discussing at length the impact and implication of adult femoral torsion.
Re: tibial torsion and your post yesterday saying that > 30deg external torsion can affect both knee and hip extension, what I still don’t understand is the mechanism behind the hip limitation. How would that torsion translate through the leg to the hip?”
There are a few things we need to remember to make sense of this:
- tibial torsion is the angular difference between the tibial plateau and distal tibial malleoli and refers only to the tibia, not the entire lower extremity (see top photo)
- pronation can occur in the rear foot, mid foot, and fore foot
- pronation causes internal spin of the leg and thigh, due to plantar flexion, eversion and abduction of the talus (see middle photo)
- internal spin of the hip causes posterior translation of the femoral head via the “glide and roll” phenomenon
- these are appropriate mechanics during the 1st ½ of the gait cycle (initial contact to mid stance)
- pronation is one of the 4 shock absorbing mechanisms (pronation, ankle dorsiflexion, knee flexion, hip flexion) of the lower extremity
now try this (yes, at home!)
- flex your knee
- internally rotate you leg
- allow your arch to flatten
- try and extend your hip
Remember these facts about supination
- supination is initiated by the swing phase leg as it starts in early swing and continues to terminal swing (see third picture)
- supination (from full pronation), should occur from midstance to pre swing
- supination makes the foot into a “rigid lever” to transpose forces from above the foot into the foot and allow for propulsion (see third picture)
- supination involves external rotation of the lower leg and thigh (see pictures 3 and 4)
- external rotation of the hip is accompanied by anterior glide of the femoral head via the “glide and roll” phenomenon
- this position puts the gluteal muscles (max and posterior fibers of the gluteus medius) at a mechanical advantage
now try this:
- extend your knee
- externally rotate your leg
- you should have a full arch at this point
- try and extend your hip
What did you (hopefully) learn?
- When the hip is in an externally rotated position it is easier to extend; the femur head moves anteriorly, the femoral joint capsule becomes tighter and stability is created
- when the hip is internally rotated, it is more difficult to extend
- the femur head glides posteriorly, changing the axis of rotation of the joint
- the gluteus maximus and posterior fibers of the gluteus medius are at a mechanical disadvantage
OK. Got it? We sure hope so! Excellent question, Matthew. Thanks for the opportunity to teach this concept.
The Gait Guys. Taking you closer to mastering the gait cycle with each post.
Podcast 70: Achilles Solutions and Foot Cases
/The Achilles and Calf: Achieve Posterior Length via Anterior Strength
A. Link to our server:
Direct Download:
http://traffic.libsyn.com/thegaitguys/pod_70final_was71.mp3
Permalink: http://thegaitguys.libsyn.com/podcast-70-0B.
iTunes link:
https://itunes.apple.com/us/podcast/the-gait-guys-podcast/id559864138
C. Gait Guys online /download store (National Shoe Fit Certification and more !) :
http://store.payloadz.com/results/results.aspx?m=80204
D. other web based Gait Guys lectures:
www.onlinece.com type in Dr. Waerlop or Dr. Allen, ”Biomechanics”
______________
Today’s Show notes:
Foot Progression Angle Exaggeration: External Tibial Torsion
Take a look at the tibial tuberosity and then where you think the 2nd metatarsal head would be. What do you see? The 2nd metatarsal is lateral to the tibial tuberosity. You are looking at external tibial torsion.
Lets see how this external tibail torsion behaves during a knee bending. Observe the medial drift of the knee during weight bearing knee flexion. Many folks would say that the problem here is the increased foot prontation, but that is not where the problem lies, that is where many of the forces are funneling though. The client is pronating more because the external tibial torsion that is creating this appearance has put the knee inside the foot tripods region of stability.
In external tibial torsion there is an external torsion or a “twist” along the length of the tibia (diaphysis or long section). This occurs in this example to the degree that the ankle joint (mortise joint) can no longer cooperate with sagittal knee joint. When taking a client with external tibial torsion and pre-postioning their foot in a relatively acceptable/normal foot progression angle there is a conflict at the knee, meaning that the knee cannot hinge forward in its usual sagittal plane. In this case with the foot progression angle smaller than what this client would posture the foot, the knee the knee will be forced to drift medially.
Are you looking for torsions of the lower limb in your clients ?
Are you forcing them into foot postures that look better to you but that which are conflicting to your clients given body mechanics ? Would you correct this client’s foot turn out (increased progression angle) ? IF you did you would likely cause them knee pain in time. Would you put them into a stability shoe to try and control the pronation ? Again, you are likely to draw their knee outside the saggital knee hinge that is presently pain free. There is more to shoe fit that just looking at the foot. First do no harm is our mantra !
Remember, telling someone to turn their foot in or out because it doesn’t appear correct to your eyes can significantly impair either local or global joints , and often both. Torsions can occur in the talus, the tibia and the femur.
Furthermore, torsions can have an impact on foot posturing at foot strike and affect the limbs loading response, from foot to core and even arm swing can be altered. Letting your foot fall naturally beneath your body does not mean that you have the clean anatomy to do so without a short term or long term cost.
This is some of the toughest stuff you will deal with clinically. The fence is narrow, if you do to little correction you fall off the fence into the wrong yard and create problems. If you do to much correction you get the same result. These torsional issues are a delicate balancing act many times. You first have to know what you have, then you have to know where the fix is, and then how much is safe. Tricky stuff. This is exactly why in some folks a stability shoe can be magic or tragic and in others dropping into zero drop minimalism can be magic or tragic.
Want more on torsion and versions ? Type the words into the search box on our blog. We have plenty of good info for you.
Shawn and Ivo, The Gait Guys
The Calcaneo Cuboid Locking Mechanism
Do you know what this is? You should if you walk or run!
It is the mechanism by which the tendon of the peroneus longus travels behind the lateral malleolus of the ankle, travels underfoot, around the cuboid to insert into the lateral aspect of the base of the 1st metatarsal and adjacent 1st cunieform (see above)
For more cool info on the peroneus longus, see our blog post here.
When the peroneus longus contracts, in addition to plantar flexing the 1st ray, it everts the cuboid and locks the lateral column of the foot, minimizing muscular strain required to maintain the foot in supination (the locked position for propulsion). Normally, muscle strength alone is insufficient to perform this job and it requires some help from the adjacent articulations.
In addition, the soleus maintains spuination during propulsion by plantar flexing and inverting rear foot via the subtalar joint. This is assisted by the peroneus brevis and tertius which also dorsflex and evert the lateral column, helping keep it locked. Can you see why the peroneii are so important?
signs of a faulty calcaneo cuboid locking mechanism
- weak peroneus longus, brevis and or tertius
- excessive rear or midfoot pronation
- low arch during ambulation
- poor or low gear “push off”
- subluxated cuboid
The calcaneo cuboid locking mechanism. Essential for appropriate supination and ambulation. Insufficiency, coming to a foot you will soon examine.
The Gait Guys. Improving your GQ (Gait Quotient) each and every day with every post we write.
Podcast 69: Advanced Arm Swing Concepts, Compensation Patterns and more
/Plus: Foot Arch Pathomechanics, Knee Pivot Shift and Sesamoiditis and more !
A. Link to our server:
http://traffic.libsyn.com/thegaitguys/pod_70ff.mp3
Direct Download: http://thegaitguys.libsyn.com/podcast-70
Permalink:
B. iTunes link:
https://itunes.apple.com/us/podcast/the-gait-guys-podcast/id559864138
C. Gait Guys online /download store (National Shoe Fit Certification and more !) :
http://store.payloadz.com/results/results.aspx?m=80204
D. other web based Gait Guys lectures:
www.onlinece.com type in Dr. Waerlop or Dr. Allen, ”Biomechanics”
______________
Today’s Show notes:
1. “Compensation depends on the interplay of multiple factors: The availability of a compensatory response, the cost of compensation, and the stability of the system being perturbed.”
What happens when we change the length of one leg? How do we compensate? Here is a look at the short term consequences of a newly acquired leg length difference.
http://www.ncbi.nlm.nih.gov/pubmed/24857934
2. Medial Longitudinal Arch Mechanics Before and After a 45 Minute Run
http://www.japmaonline.org/doi/abs/10.7547/12-106.1
3. Several months ago we talked about the pivot-shift phenomenon. It is frequently missed clinically because it can be a tricky hands on assessment of the knee joint. In this article “ACL-deficient patients adopted the … .* Remember: what you see in their gait is not their problem, it is their strategy around their problem.
http://www.clinbiomech.com/article/S0268-0033(10)00264-0/abstract
4.Do you know the difference between a forefoot supinatus and a forefoot varus?
"A forefoot varus differs from forefoot supinatus in that a forefoot varus is a congenital osseous deformity that induces subtalar joint pronation, whereas forefoot supinatus is acquired and develops because of subtalar joint pronation. ”
http://www.ncbi.nlm.nih.gov/pubmed/24980930
5. Pubmed abstract link: http://www.ncbi.nlm.nih.gov/pubmed/24865637
Gait Posture. 2014 Jun;40(2):321-6. Epub 2014 May 6.
Arm swing in human walking: What is their drive?
Goudriaan M, Jonkers I, van Dieen JH, Bruijn SM
6. This is Your Brain On Guitar
http://www.the-open-mind.com/this-is-your-brain-on-guitar/
So you want to do a Gait Analysis: Part 4
This is the 4th in a multi part series. If you missed part 1, click here. For part 2, click here, part 3, click here.
These are the basics, folks. We hope this is a review for many.
A quick review of the walking gait cycle components:
There are two phases of gait: stance and swing.
Stance consists of:
- Initial contact
- Loading response
- Midstance
- Terminal stance
- Pre-swing
Swing consists of:
- initial (early) swing
- mid swing
- terminal (late) swing
today, lets explore Terminal stance
Terminal stance is one of the last stages of stance phase. Following midstance, where maximal pronation should be occurring, the stance phase foot should now begin supinating, initiated by the the opposite foot in swing phase moving forward of the center of gravity.
Lets look at what is happening here at the major anatomical areas:
Foot
- Supination begins from the opposite, swing phase leg (see above)
- the calcaneus inverts to neutral
- the center of gravity of the foot raises from its lowest point at midstance
- The lower leg should begin externally rotating (as it follows the talus)
- The thigh should follow the lower leg and should also be externally rotating; sometimes to a greater extent due to the shape and size of the medial condyle of the femur (which is larger than the lateral)
- these actions are perpetuated by the gluteus maximus and posterior fibers of the gluteus medius, as well as posterior compartment of the lower leg including the flexor digitorum longus, flexor hallucis longus, peroneus longus and tibialis posterior
- The ankle should be 5 degrees dorsiflexed and in ankle rocker
- the calcaneocuboid locking mechanism should be engaging to assist the peroneus longus in getting the head of the 1st metatarsal to the ground
Knee
- near or at full extension. This is perpetuated by the quadriceps and biceps femoris, contracting concentrically and attenuated by the semi membranosis and tendonosis. The popliteus contracts eccentrically as soon as the knee passes midstance to keep the rates of external rotation of the tibia and femur in congruence.
Hip
- The hip should be extending to 10 degrees.
Can you picture what is happening? Try and visualize these motions in your mind. Can you understand why you need to know what is going on at each phase to be able to identify problems? If you don’t know what normal looks like, you will have a tougher time figuring out what is abnormal.
Ivo and Shawn. Gait and foot geeks extraordinaire. Helping you to build a better foundation to put all this stuff you are learning on.
pictured used with permission from Foot Orthoses and Other Conservative Forms of Foot Care
Subtle Clues to Ankle Rocker Pathology: How good are your powers of observation ?
There are clues showing you there is motor pathology to ankle dorsiflexion, if you are paying close enough attention.
When we see motor pathology in ankle dorsiflexion we immediately begin to think about impairment to hip extension range of motion, gluteal strength, motor coordination and many other issues.
Here is a simple case. Observation skills are your greatest superpower when it comes to figuring out many gait and movement problems. But, you have to know what to look for and know what they mean before you can even hope to know how to fix things.
This is a simple video. It shows active ankle dorsiflexion in supination. We asked the client (a runner with right heel and persistent sesamoid pain following a healed sesamoid fracture) to perform simple ankle dorsiflexion. This is what we saw.
It should be clear to the observer that the end of the video shows attempted right dorsiflexion pulls the 2-5 toe extensors into the pattern quite aggressively and as a dominating faction. One can see toe abduction and extension with surprisingly little help from the long hallux toe extensor (EHL). Dorsiflexion also fatigued early on the right. There is only one reason that the lesser toe extensors (EDL & EDB) are being over recruited, it’s because the EHL and tibialis anterior are weak and/or inhibited or have been pattern corrupted for one reason or another. Depending on this smallest of anterior compartment muscles over the EHL and tib anterior will mean that ankle rocker (dorsiflexion) is impaired. It also means that abnormal forefoot valgus posturing is expected (we could make a case for valgus or varus depending on other variables present). Passive ROM assessment confirmed the impaired ankle rocker with barely greater than 90 degrees ankle dorsiflexion ROM. This impairment will possibly do many things including:
- premature heel rise
- premature gastrocsoleus engagement
- accentuated rear foot eversion (Rearfoot pronation)
- midfoot pronation
- strain of plantar fascia
- premature forefoot loading response (strong clue for clients sesamoid fracture and persistent pain)
- anterior/ posterior shin splints
- hallux VALgus /bunion formation
- long toe flexor dominance and many other things.
This clinical find plays nicely into the clients multiple symptoms (plantar pain and sesamoid problems) and functional gait pathology.
Restoring proper motor hierarchy and synchrony to the ankle dorsiflexion team (tib anterior, peroneus tertius, EDL, EHL) will reduce the need for solitary group overuse and impart forces where they should be when they need to be present. Impair the synchrony and problems ensue.
Help your client achieve the motion at the ankle mortise and they do not have to pass the buck into the foot. Always test for skill, endurance and strength. Endurance is the most often forgotten assessment. If endurance is lost early, the brain will begin to block out that end range of motion because it cannot be trusted, and thus posterior compartment tightness will be detected. This is an often common source of regional achilles and para-achilles tendonopathy. If your clients symptoms take time during activity to develop looking at the endurance of motor patterns may give the clue to your solution.
Simple case, but you have to know your normal gait parameters, know functional anatomy and know how impaired mechanics factor into injury.
Shawn and Ivo
The gait guys
Spine pain and arm swing. Do you truly get this ? You had better.
We have all seen that runner who swings the one arm more than the other, they may even violently thrust the one arm across the front of the torso. If you have been a spectator half way through any race you have seen this person. And, if you are watching carefully in your gym, lab, office or gait lab you have seen the accentuated arm swing on one side (or is it the loss of arm swing on the opposite, we discussed some of these games in last weeks blog post here). You have also see the person who is running with a water bottle in their hand and altering their neurological arm-leg swing opposite pairing and thus their anti-phasic shoulder-pelvic girdle pairing (see attached photo). (If you are lost when we discuss the terms phasic and anti-phasic you will want to go and read this previous blog post.)
Knowing that which you are seeing in your client is their highest level of neurologic motor compensation, and not likely their problem, represents a higher thought process in a diagnostician. Unfortunately, it also opens a whole bunch of clinical thought process mental gymnastics.
Our purpose of today’s blog post is to revisit an important aspect of the clinical examination, observation. Listening and watching (and knowing what you are seeing, and not seeing) are two of the biggest pieces of a clinical exam other than the hands on assessments. One has to be good at all of the pieces. But then their is the knowledge base that is needed to base the information and choices upon so that the proper path to remedy can be chosen. Without the knowledge the actions and choices can be dramatically incorrect and devastating to an athlete or client/patient. Make the wrong choice for a patient and they do not get better, perhaps even get worse. Make the wrong choice for an athlete and you deepen their compensation and increase their risk for injury. This is one of our pet peeves because we recognize that we have a deep knowledge base and yet we find ourselves without the certainty and answers on a regular basis and yet we see people making similar choices for clients and athlete with only a small piece of the knowledge necessary on their table to make those choices. If you don’t know what you don’t know, and yet your still swimming in the risky waters, you are already in deep trouble.
Here are two articles that you should be familiar with. We talk about them in depth in our “arm swing” online course #317 here. These articles talk about phasic and antiphasic motions of the arms and shoulder-pelvic blocks. They talk about spine pain and how spine pain clients reduce the antiphasic rotational (axial) nature of the shouder girdle and pelvic girdle. They elude to the subcortial pattern of choice to rotate them as a solid unit to reduce spine rotation, axial loading and compression and that spine pain disables the normal arm-leg pendulums. If you do not know and understand these principles, and you are training, treating or coaching people, you are a problem waiting to happen for your client. You, are the problem and your choices could likely hurt your client. IF you do not know how to address them or fix them safely, it is your job to send them to someone who does.
So the next time you see an aberrant arm swing, during your exam, your observations and your history better delve into all things relevant. How about that 20 year “healed” ankle fracture that your client dismisses as “oh, but that was 20 years ago, its not part of this problem i am having now”. How about that episode of frozen shoulder that was “fixed” 15 years ago or that episode of hip or knee pain from falling on ice or the random big toe pain or the headaches ? If they dismiss all of this because they are just coming to see you for spine pain or because their running partner says their arm swing stinks on the right you had better sit down for a longer ride, because you know better now. Unless you prefer to see life through tunnel vision. Sure it is easier, but don’t you want more for your client ?
Sorry for the rant.
Shawn and Ivo, …… the gait guys.
Mechanical coupling between transverse plane pelvis and thorax rotations during gait is higher in people with low back pain.
You can only “borrow” so much before you need to “pay it back”
How can feet relate to golf swing?
This 52 year old right handed gentleman presented with pain at the thoracolumbar junction after playing golf. He noticed he had a limited amount of “back swing” and pain at the end of his “follow through”.
Take a look a these pix and think about why.
Hopefully, in addition to he having hairy and scarred legs (he is a contractor by trade), you noted the following
- Top left: note the normal internal rotation of the right hip; You need 4 degrees to walk normally and most folks have close to 40 degrees. He also has internal tibial torsion.
- Top right: loss of external rotation of the right hip. Again, you need 4 degrees (from neutral) of external rotation of the hip to supinate and walk normally.
- Top center:normal internal rotation of the left hip; internal tibial torsion
- 3rd photo down: limited external rotation of the left hip, especially with respect ti the amount of internal rotation present; this is to a greater degree than the right
- 4th and 5th photos down: note the amount of tibial varum and tibial torsion. Yes, with this much varum, he has a forefoot varus.
The brain is wired so that it will (generally) not allow you to walk with your toes pointing in (pigeon toed), so you rotate them out to somewhat of a normal progression angle (for more on progression angles, click here). If you have internal tibial torsion, this places the knees outside the saggital plane. (For more on tibial torsion, click here.) If you rotate your extremity outward, and already have a limited amount of range of motion available, you will take up some of that range of motion, making less available for normal physiological function. If the motion cannot occur at the knee or hip, it will usually occur at the next available joint cephalad, in this case the spine.
The lumbar spine has a limited amount of rotation available, ranging from 1.2-1.7 degrees per segment in a normal spine (1). This is generally less in degenerative conditions (2).
Place your feet on the ground with your feet pointing straight ahead. Now simulate a right handed golf swing, bending slightly at the waist and rotating your body backward to the right. Now slowly swing and follow through from right to left. Note what happens to your hips: as you wind back to the right, the left hip is externally rotating and the right hip is internally rotating. As you follow through to the left, your right, your hip must externally rotate and your left hip must externally rotate. Can you see how his left hip is inhibiting his back swing and his right hip is limiting his follow through? Can you see that because of his internal tibial torsion, he has already “used up” some of his external rotation range of motion?
If he does not have enough range of motion in the hip, where will it come from?
he will “borrow it” from a joint more north of the hip, in this case, his spine. More motion will occur at the thoracolumbar junction, since most likely (because of degenerative change) the most is available there; but you can only “borrow” so much before you need to “Pay it back”. In this case, he over rotated and injured the joint.
What did we do?
- we treated the injured joint locally, with manipulation of the pathomechanical segments
- we reduced inflammation and muscle spasm with acupuncture
- we gave him some lumbar and throacolumbar stabilization exercises: founders exercise, extension holds, non tripod, cross crawl, pull ups
- we gave him foot exercises to reduce his forefoot varus: tripod standing, EHB, lift-spread-reach
- we had him externally rotate both feet (duck) when playing golf
The Gait Guys. Helping you to store up lots “in your bank” of foot and gait literacy, so you can help people when they need to “pay it back”, one case at a time.
Podcast 68: Gait , Arm Swing, Neuro-developmental Windows
/A. Link to our server:
Direct Download: http://traffic.libsyn.com/thegaitguys/pod_68ffinal.mp3
Permalink: http://thegaitguys.libsyn.com/podcast-68
B. iTunes link:
https://itunes.apple.com/us/podcast/the-gait-guys-podcast/id559864138
C. Gait Guys online /download store (National Shoe Fit Certification and more !) :
http://store.payloadz.com/results/results.aspx?m=80204
D. other web based Gait Guys lectures:
www.onlinece.com type in Dr. Waerlop or Dr. Allen, ”Biomechanics”
______________
Today’s Show notes:
1.Brain implant helps paralysed man move his hand
http://realitysandwich.com/220399/brain-implant-helps-paralysed-man-move-his-hand-wired-uk/?u=95820
2. Has Science Finally Confirmed the Existence of Acupuncture Points, Validating Chinese Medicine?
“Shoes affect the gait of children. With shoes, children walk faster by…
Arm Swing Truths, and Lies.
We have been reminded over and over again in recent weeks how intimately arm swing is tied to leg swing. We have recently had clients in our practices with strokes (ischemic and hemorrhagic), transverse myelitis, inflammatory neurologic disorder and the plethora of biomechanically pain-mediated gait responses affecting the limbs, including the upper limbs which manifest many variations in these people’s normal gait neuro-mechanics.
We are even reminded of the recent triathlete who had a right hip weakness that was allowing him to drift into the right frontal plane in running and biking. Upon asking about further symptoms he mentioned left hand tingling on longer bike training rides. We asked if he recalled sliding/shifting onto the right side of the saddle/seat often to find power in the right leg and he mentioned matter of fact that it is a constant awareness. We then suggested that he was having to over pressure into the left handle grips to keep the bike on a straight line because of the right pelvis-saddle shift. He was wide eyed and shocked that it was what he was in fact aware of. Moral of the story: even in on the bike opposite arm and leg action are intimately tied together. After testing and assessment it was clear that a function TOS (thoracic outlet syndrome) was in effect because of shortness and increased tone in the left pectoral chest wall compromising neurovascular bundle compression and generating hand paresthesias (numbness/tingling). A simple fix if you fix the right pelvic frontal plane drift. If you try to fix the TOS at the shoulder-neck level resistance to progress is likely.
Arm swing is a sneaky thing. There are many variables. We have discussed many of these arm swing variables in 38 previous blog posts (link here) and we have whole lecture here on arm swing (this slide is part of that in depth lecture).
In the pubmed article below there is new research delving into passive and active components of arm swing. There are both, clearly. But what a reader needs to take away is that a clinical examination must be part of every assessment to discover the active components (muscular and neuromuscular) that are missing (ie. weak posterior deltoid, lat dorsi etc) and which need fixing and rehabilitation and the passive components that are inhibitory to the big picture (mobility, stability).
It should be clear by now, if you have been with us for at least the last year, that what you see in someone’s gait is their compensation, not their problem. Addressing resolution measures to change what you see is a path to deepening the compensation or developing others. Arm swing is intimately tied to the lower limbs, and powerfully so to the opposite leg. A deficit in the leg will be expressed in some way in the opposite upper limb, which in turn forces a compensatory change in the opposite upper limb and thus down into the “other” opposite lower limb. One thing affects many. The wrong intervention drives bigger problems, so make sure you know your gait “normal” parameters and be sure a clinical examination is a huge part of your discovery toward the answers for your client.
Shawn and Ivo … . . the gait guys
Pubmed abstract link: http://www.ncbi.nlm.nih.gov/pubmed/24865637
Gait Posture. 2014 Jun;40(2):321-6. Epub 2014 May 6.
Arm swing in human walking: What is their drive?
Abstract
The results confirm that passive dynamics are partly responsible for arm swing during walking. However, without muscle activity, passive swing amplitude and relative phase decrease significantly (both p<0.05), the latter inducing a more in-phase swing pattern of the arms. Therefore, we conclude that muscle activity is needed to increase arm swing amplitude and modify relative phase during human walking to obtain an out-phase movement relative to the legs.
Flat Dogs
Take a look at these pedographs. Wow!
- No rear foot heel teardrop.
- No midfoot arch on left foot and minimal on right.
- An elongated 2nd metatarsal bilaterally and forces NOT getting to the base of the 1st metatarsal and stalling on the 2nd: classic sign of an uncompensated forefoot varus.
- increased printing of the lateral foot on the right
Knowing what you know about pronation (need a review? click here) Do you think this foot is a good lever? Do you think they will be able to push off well?
What can we do?
- foot exercises to build the intrinsic and extrinsic muscles of the foot (click here, here, here, and here for a few to get you started)
- perhaps an orthotic to assist in decreasing the pronation while they are strengthening their foot
- motion control shoe? Especially in the beginning as they are strengthening their feet and they fatigue rather easily
The prints do not lie. They tell the true story of how the forces are being transmitted through the foot. For more pedograph cases, click here.
The Gait Guys. Teaching you more about the feet and gait. Spreading gait literacy throughout the net! Do your part by forwarding this post to someone who needs to read it.
The weeping calf and the deconstructed arm swing.
Last week we showed you this video and blog post of a compressive left lower leg neuropathy and what it looks like when both heel and toe walking are attempted when both are compromised. It was nothing exciting but to see both in a clinical presentation is not all that common.
In today’s videos (the one above and this one here), the videos were all shot on the same day incidentally, we wanted you to see this gentleman’s gait in it’s normal gait pattern attempt. Because less of the extremes of range and strength are required, it is far more difficult to detect the issues than in last week’s video clip (here).
There are plenty of things to talk about in this video but lets just point out one of them here today. Remember, the lesion is in the left lower leg.
Absent right arm swing.
We have been harping about arm swing for a long time. Go to the search box here on our blog and type in “arm swing” and you will find an abundance of articles on the biomechanics and neurology of arm swing and how it is tied to leg swing. In this case we have foot drop and impaired calf raise (video link) on the left. Their function is impaired/depressed. We are seeing this matching in the absence of right upper limb swing. Remember, most of the time the upper limb takes the queue from the opposite lower limb. This is why coaching arm swing changes is not a sound idea most of the time, look for functional opportunities for changes in the opposite lower limb if deficits are present there.
Part of what you are seeing is the increased activity in the left arm swing. Why ? Because the client is abruptly lurching off of the left leg because of the stability and strength deficits in that limb. The brain knows that bearing weight on the left limb has challenges. This causes an abrupt pitch (early departure) forward onto the right leg and this will be met with increased left arm swing (go limb around your home or office, you will see that it is a coupled phenomenon). So, is it increased left arm swing you are seeing because of this issue we just mentioned or are you seeing decreased right arm swing because of the matching neuro-suppression of left leg ?
This is where your clinical examination must come into play. Shame on anyone that is making the changes without clinical information. One must see that there rare two (at least) possible scenarios for the differential in arm swing. And one must also see that the arms in this case are not the issue, that it is the left lower limb deficits that are driving the issue. Guaranteed.
Arm swing……..more to it than you might think.
Shawn and Ivo, The gait guys