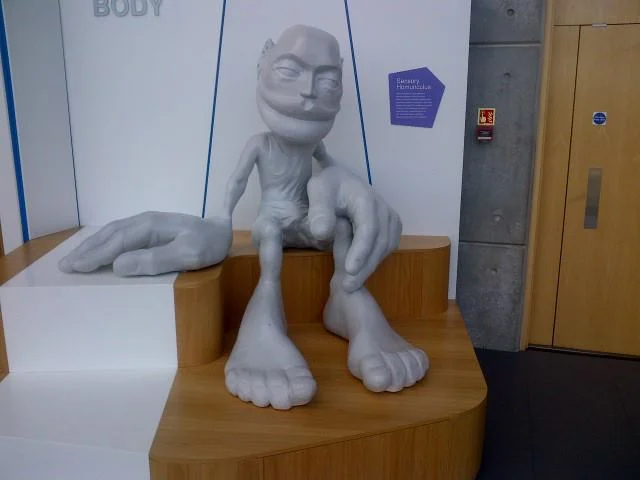
The EHB....In all its glory...
/The extensor hallucis brevis : An overlooked "miracle worker"
The Extensor Hallicus Brevis, or EHB as we fondly call it is an important muscle for descending the distal aspect of the 1st ray complex (1st metatarsal and medial cunieform) as well as extending the 1st metatarsophalangeal joint. It is in part responsible for affixing the medial tripod of the foot to the ground. Its motion is generally triplanar, with the position being 45 degrees from the saggital (midline) plane and 45 degrees from the frontal (coronal) plane, angled medially, which places it almost parallel with the transverse plane. With pronation, it is believed to favor adduction (1).
It arises from the anterior calcaneus and inserts on the dorsal aspect of the proximal phalynx. It is that quarter dollar sized fleshy protruding, mass on the lateral aspect of the dorsal foot. The EHB is the upper part of that mass. It is innervated by the lateral portion of one of the terminal branches of the deep peronel nerve (S1, S2), which happens to be the same as the extensor digitorum brevis (EDB), which is why some sources believe it is actually the medial part of that muscle. It appears to fire from loading response to nearly toe off, just like the EDB; another reason it may phylogenetically represent an extension of the same muscle (2-4).
Because the tendon travels behind the axis of rotation of the 1st metatarsal phalangeal joint, in addition to providing extension of the proximal phalynx of the hallux (as seen in the child above), it can also provide a downward moment on the distal 1st metatarsal (when properly coupled to and temporally sequenced with the flexor hallicus brevis and longus), assisting in formation of the foot tripod we have all come to love (the head of the 1st met, the head of the 5th met and the calcaneus).
Why is this so important?
The central axis of a joint (sometimes called the instantaneous axis of motion) is the center of movement of that articulation. It is the location where the motion will occur around, much like the center of a wheel, where the axle attaches. In an articulation, it usually involves one bone moving around another. Lets look at an example with a door hinge.
A hinge is similar to a joint, in that it has parts with is joining together (the door and the jamb), with a “joint” in between, The axis of rotation of the hinge is at the pivot rod. When the door, hinge and jamb are all aligned, it functions smoothly. Now imagine that the hinge was attached to the jamb 1/4” off center. What would happen? The hinge would bind and the door would not operate smoothly.
Now let’s think about the 1st metatarsal phalangeal joint. It exists between the head of the 1st metatarsal and the proximal part of the proximal part of the proximal phalanyx. Normally, because the head of the 1st metatarsal is larger than the heads of the lesser ones, the center of the joint is higher (actually,almost 2X as high; 8mm as opposed to 15mm). We also remember that the 1st metatarsal is usually shorter then the 2nd, meaning during a gait cycle, it bears the brunt of the weight and hits the ground earlier than the head of the 2nd.
The head of the 1st metatarsal should slide (or should we say glide?) posteriorly on the sesamoids during dorsiflexion of the hallux at pre swing (toe off). It is able to do this because of the descent of the head of the 1st metatarsal, which causes a dorsal posterior shift of the axis of rotation of the joint. We remember that the head of the 1st descends through the conjoined efforts of supination and the coordinated efforts of the peroneus longus, extensor hallucis brevis, extensor hallucis longus, dorsal and plantar interossei and flexor hallucis brevis (which nicely moves the sesamoids and keeps the process going smoothly)(1, 5).
Suffice it to say, if things go awry, the axis does not shift, the sesamoids do not move, and the phalanyx crashes into the 1st metatarsal, causing pain and if it continues, a nice spur you can write home about!
Treating and needling this muscle is easy, as it is very accessible on the dorsum of the foot and due to the decreased receptor density, is not too uncomfortable. We like to needle the peroneus longus and short flexors as well, as they all have the function of lowering the head of the 1st ray. Check it out in this quick how to video.
1. Michaud T: Human Locomotion: The Conservative Management of Gait Related DisordersNewton Biomechanics; First Edition 2011
2. https://www.physio-pedia.com/Extensor_Hallucis_brevis
3. http://www.wheelessonline.com/ortho/extensor_hallucis_brevis
4. Becerro de Bengoa Vallejo R., Losa Iglesias M.E., Jules K.T. Tendon Insertion at the Base of the Proximal Phalanx of the Hallux: Surgical Implications (2012) Journal of Foot and Ankle Surgery, 51 (6) , pp. 729-733.
5. Zelik, K.E., La Scaleia, V., Ivanenko, Y.P. et al. Eur J Appl Physiol (2015) 115: 691. https://doi.org/10.1007/s00421-014-3056-x