A novel way to look at functional internal rotation of the hips
/As clinicians (and coaches) we are often trying to figure out different ways to functionally assess internal rotation of the hips. How many times does the patient/client “appear“ to have appropriate internal rotation on the table only to find out that they don’t functionally and vice versa.
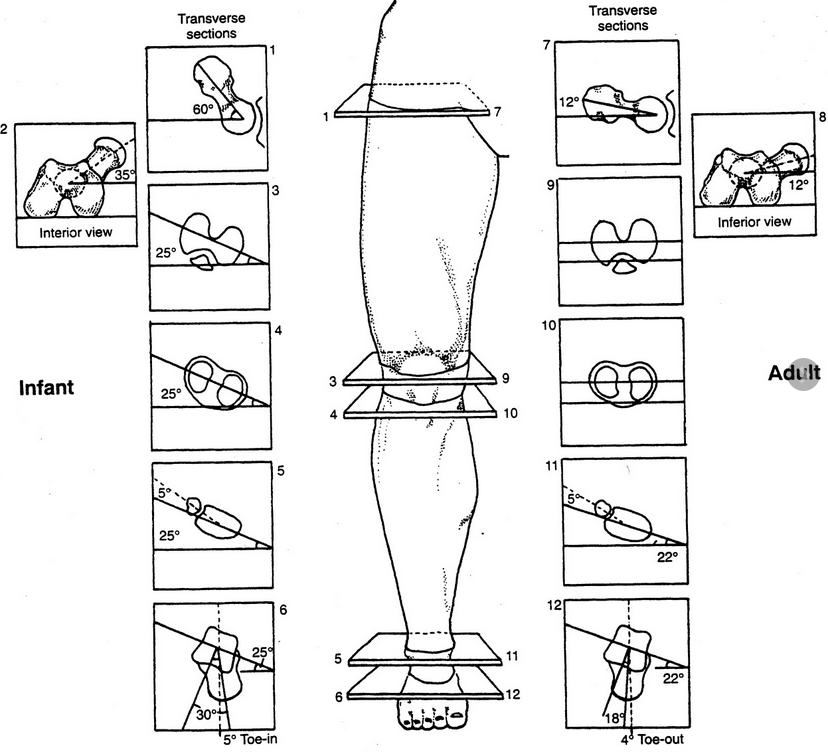
Take a look at it this gentleman who is a ski instructor. We are trying to simulate the standard side to side ski motion in a way that would be functionally appropriate. Keep in mind that he has bilateral internal tibial torsion and bilateral femoral retro torsion. When he began care at our office he had 5° external rotation on the right and about 8° external rotation on the left as his FULL AMOUNT OF INTERNAL ROTATION AVAILABLE to him bilaterally.
Treatment consisted largely of hip mobilization, Therapeutic exercises to emphasize internal rotation of the hips such as hip helicopters, airplanes and supine “chairs“ with internal rotation and adduction utilizing a ball between the knees; we also did acupuncture/needling of the hip capsules as well as anterior fibers of the gluteus medius and minimus. He now has about 5° internal rotation on the right now and a little less than 5 on the left. Note how the motion is clearly visualized in this video below.
Do you have other novel ways to test internal rotation of the hips functionally? Leave a comment or drop us a line and let us know
Feel like you want more? Join us this Wednesday evening on onlinece.com for Biomechanics 326: 6 MST
Dr Ivo Waerlop, one of The Gait Guys.
#functionaltesting #functionalmovement #hip #internalrotation #femoralretrotorsion #femoralretroversion #thegaitguys