Imposter syndrome and careful what you say, and read.
/Why most published research findings are false.
Ioannidis JP1.
PLoS Med. 2005 Aug;2(8):e124. Epub 2005 Aug 30.
"Simulations show that for most study designs and settings, it is more likely for a research claim to be false than true. Moreover, for many current scientific fields, claimed research findings may often be simply accurate measures of the prevailing bias. In this essay, I discuss the implications of these problems for the conduct and interpretation of research."
Artwork:
from what we can tell, a rework of @rundavidrun artwork, reworked by @MatthewJDalby. Thank you gentlemen.
People received an incomplete picture from a small slice of a clinical exam pie yesterday and made some bold , yet reasonable judgements admittedly. We admit they are germane points and arguments, though easily biased on this small slice video, and unfair in the bigger picture. I will always back Ivo, he is one of the smartest clinicians i know, and if you have listened to our podcast it should be clear to anyone that he can run circles around most with his deep well of knowledge. Dr. Ivo showed a video that discussed some of the things he likes to consider on an exam, not his entire exam, to discuss some things he likes to think about and incorporate into his exam sometimes, things that have become reliable patterns that work for him in practice. Many of us have gone through these exam methods at one time if we have been in the fields long enough, and many of us know that "i do not feel a darn thing that they say i am supposed to" BUT, when put into a full complete exam, for Ivo, these things meshed with other exam inputs honed over a 25+ year history in the field mean something to him. And bottom line, results speak. That is all that matters because a lot of research is often full of holes. I too have some old tricks in my bag that are admittedly somewhat unsupported, but in a bigger picture when all the exam intake variables are brought together, decades of experience allow us to use deeper clinical experience to bring forth some ideas on the client's pain and problems. If we were all to abandon all of our older tricks that have proven valuable, who suffers ? And for what? a few studies that question validity? Everyone's educational past is full of holes and ignorance that has been disproven (yes, even your high school physics knowledge has been rewritten, but it does not mean that the broader insights that have grown from said knowledge is wrong. For example, even today's Low back pain research is becoming more and more untenable in some studies as to the true source of the pain, this has been a huge topic of discussion on some forums by very intelligent people. We are all reading small pieces of new research that tell us "this thing" or that thing is of low reliabilty and we question ideas of old. Some new research is now suggesting that ACL tears do not need surgery, so do we just stop doing ACL repairs? No, that is foolish, but just because the new doesn't support the old doesn't mean the old is useless and without clinical value. Here is what matters, can you help the person in front of you ? That is what matters. How you assess and go about it is not what matters to your patient. Ivo is top shelf, period. There are few people that have the depth and breadth of his knowledge in neurology and if you knew his depth of physiology was even deeper you'd be fully blown away. Listen to one of our podcasts if you do not believe me, he can run circles around me, for what little that might be worth. Productive comments can be made to create a debate without being snide. You only show you are a turd and your true colors (brown) when you cannot be professional. We work hard here, if you can't be professional, go somewhere else, please.
Oh, and still want to question things, good, you should, we all should. So, here, question EVERYTHING then.
Then again, there are those that will question this too, as they should. And so, if we just left our selves to decide to only use things deemed valid per today's thin research standards (what is your predatory journal count up to these days?) , then we dismiss much of what we used in our past that we used to actually help people. Do i dare ask those slinging stones to remember this post when 20 years from now the then research might dismiss many of the things they presently deem "law" and solid research?
Bottom line, judge softly, with open eyes, a touch of wisdom and skepticism, and self honesty in the knowledge that much of what we do, and think we do, is also rubbish, but sometimes yet still seems to help people.
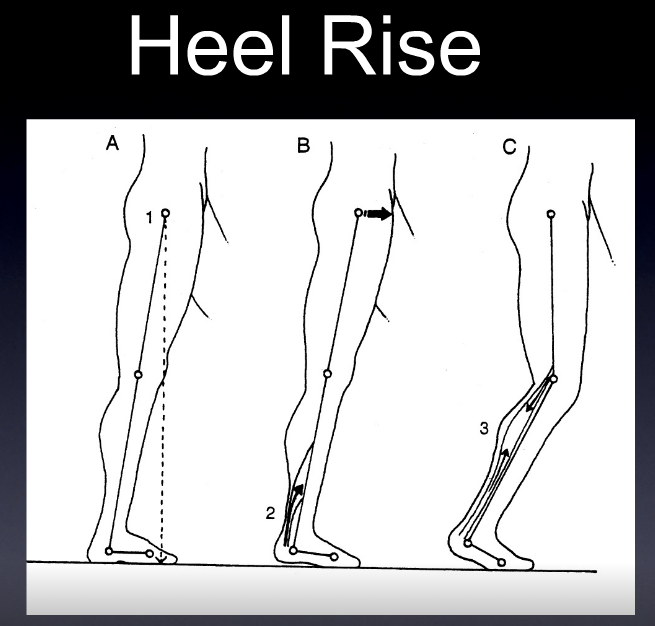
And for those who still think they know it all, look at today's art work.
Shawn Allen, humble partner of a wise man, wiser than most. Dr. Ivo
PLoS Med. 2005 Aug;2(8):e124. Epub 2005 Aug 30.
Why most published research findings are false.
Ioannidis JP1.
"Simulations show that for most study designs and settings, it is more likely for a research claim to be false than true. Moreover, for many current scientific fields, claimed research findings may often be simply accurate measures of the prevailing bias. In this essay, I discuss the implications of these problems for the conduct and interpretation of research."
Comment in
Modeling and research on research. [Clin Chem. 2014]
The clinical interpretation of research. [PLoS Med. 2005]
Minimizing mistakes and embracing uncertainty. [PLoS Med. 2005]
Truth, probability, and frameworks. [PLoS Med. 2005]
Power, reliability, and heterogeneous results. [PLoS Med. 2005]
Why most published research findings are false: problems in the analysis. [PLoS Med. 2007]
When research evidence is misleading. [Virtual Mentor. 2013]
The Value of P. [Am J Transplant. 2016]
https://www.ncbi.nlm.nih.gov/pubmed/16060722