Compressing the Distal Tib-Fib joint. Really ?!
If you do not know your biomechanics, this could be a road to problems for your client.
Many who viewed this video will not know the “Caveat emptor” we will expand upon below.
Here is the meat of today’s blog post:
The distal tibia-fibular syndesmosis is supposed to separate during ankle dorsiflexion to accommodate for the wider ankle mortise anteriorly, compressing the two bones could nullify this range.
There are new ideas on the web every day; through new ideas come new innovations. These bands (some call them Voodoo bands) are all the rage right now, and they may have value depending on their use (and the wisdom of the user), but from what we can tell even the innovators are at a bit of a loss as to what the heck is truly happening with their use. All we have right now is theories, but understandably things have to start somewhere. We propose some logical thoughts on this video implementation here today.
Some people are using the bands over larger muscle masses, perhaps using the compression and shear between tissue layers to act as a kind of “flossing” or “active release” to the muscle and myofascia. The goal seems mostly to gain more joint range and thus greater function through that joint. Some think the vascular/ischemic challenge is creating partial effects. Others appear to be using the band to change joint compression to change stability to change mobility. We suspect others are using them to manage joint shear, we hope they realize they are impacting that component. One must keep in mind that a joint that is cylindrically compressed (such as in the video) and then subsequently loaded may still undergo motion and shear at the opposing joint surfaces. The question is, are you getting what you want? The even bigger question is have you the earned stability on that new mobility if you are about to go add activity on this new range? New “borrowed” range, meaning mobility that has been acquired but not been earned via the muscles that were supposed to achieve and maintain it, may be a recipe for injury risk. One must also not forget that with a primary motion there is an accessory motion (ie. roll and glide are in opposite directions for concave/convex joint relationships). This is a concept of joint centration, and when there is excessive uncontrolled shear there cannot be adequate centration. Too much axial compression may limit primary motion while minimizing shear but could impact accessory motion, a mulit-edged sword. There is really no good and certain way to do all this except intrinsically via the muscles surrounding the cylinder. Any extrinsic attempts must be met with the realization and understanding of the true mechanics of compression, shear, primary motion and accessory motions. So just keep in mind that things like impingement, shear and peripheral joint loading (as opposed to centrated loading) are risk factors when these components are not well understood.
That all said, we bring these concerns to light today in regards to the above mobilization video. Many who viewed this video will not know the “Caveat emptor” we have eluded to above and will expand upon below. That caveat should have (in our opinion) been mentioned. We are not trying to pick on folks, trolling or being pricks, we know everyone is just trying to help contribute to the mass knowledge base here on the web but one has to understand biomechanics in order to deliver a clean honest method without tipping the risk reward scale. We think our caveat is very much worth mentioning so that the knowledge is available to everyone. We bet the doctor in the video knows all about what we are writing here today, but many others will not, and so by debating and critiquing we all raise the bar, for the good of all mankind. In turn, we expect the same critique should happen to our material, after all, the collective mind is more powerful than the individual mind.
Here is the meat of today’s blog post:
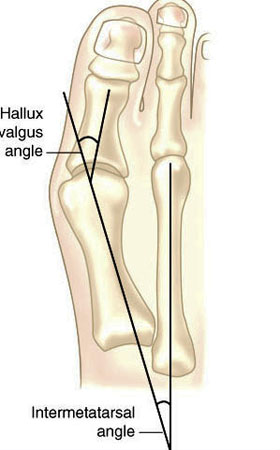
The distal tibia-fibular syndesmosis is supposed to separate during ankle dorsiflexion to accommodate for the wider ankle mortise anteriorly. More gently stated, as dorsiflexion progresses at the ankle mortise complex, the distal tibia-fibula must be able to change to accept the wider anterior mortise engagement. This is normal ankle biomechanics, for everyone ! So, why would you want to compress the distal tib-fib and attempt at arresting or limiting the normal spreading process during ankle dorsiflexion? What about the ligamentous structures that depend upon clean terminal dorsiflexion and congruent tib-fib-mortise orchestration ? Cylindrical compression could impair or limit terminal dorsiflexion range. Wasn’t this the purpose of the mobilization in the first place? This mobilization is just not something that we will be recommending you start tossing out in your rehab or training room unless you can justify on a case by case basis a reason for possibly working against normal clean biomechanics, unless of course you are sure to stay within reasonable compression limits. If you compress these bones too much, you are potentially creating mid or end range joint impingement.
We are sure the argue point will be that the band is not applied tightly enough to create sufficient compression to limit this normal range. This may be true. But,
- “Think of how stupid the average person is, and realize half of them are stupider than that.” -George Carlin
All joking aside now, but for the “average Joe” who might think that more is better, our caveat is worthy in our opinion especially when you see the volume of band used in some other videos.
SIDEBAR: Dear Gait Guys brethren, as members of those on the web who are supposed to know better, we all have a responsibility to act and portray truth and accuracy to those that are not in our lines of profession and knowledge. There are videos on line demonstrating a cavalier approach to using these bands (we are not at all referring to today’s video), we beg you to think about who is seeing these videos, possibly herds of runners and athletes looking for quick answers to their problems. Know that you may be the first line of intervention to help direct these folks to an informed way to implement self-treatment.
Back to the video for one final point.
We see that after some cylinder compression is rendered by the band, as terminal ankle dorsiflexion is mobilized we see end range mobilizing of internal and external rotation. Remember, if the compression is too much (and again, it may not be in this case if band tension application is reasonable), as dorsiflexion is attempted we will have more closed pack-type joint compression binding mid-range, and this may mean risk to articular cartilage. Just something to keep in mind. Listen to your client feedback when they do this or you instruct them, pain is obviously not a welcome outcome when you are performing potentially impinging therapies.
Here on The Gait Guys we previously shared our mnemonic , “anterior strength achieves posterior length to drive ankle dorsiflexion range”. That does not in any way mean that mobilizations are not worthy efforts at any time during a treatment. As a clinician, sometimes you have to address the tissue length of the posterior compartment tissues, but if that is not the primary cause of loss of dorsiflexion you are commissioned to look elsewhere. Also, remember that ankle dorsiflexion can be disguised through foot pronation and this in itself can enable pathology. This is perhaps one of the biggest omissions in ankle dorsiflexion mobilization videos across the board.
Make no mistake, you can mobilize all you want but at the end of the day you must improve skill, endurance and strength (S.E.S.) as well as functional stability and capacity on these new patterns of mobility if you are to do your client justice. Failure to do these things will result in loss of the gained mobility and risk for injury. Almost anyone can gain more joint motion, we have all been doing this various ways for decades. Can you earn enough capacity to keep the new mobility on a clean and correct motor pattern without corruption is the bigger question. Remember, just because you force a joint range, as opposed to earning it, doesn’t mean it is wise. Try this logic on any adhesive capsulitis shoulder patient, you will surely receive a five finger death punch in return.
There is much in the way of innovation and free thinking out there today and everyday the internet opens our collective eyes and minds to new ideas and possibilities. We all must keep in mind that many of these new things are in their infancy, some will survive with validation and some will wither away without it. It is up to the practitioner to take their client’s case to heart, do the best they can with the knowledge they have, accept when their scope of knowledge and practice has been met, and always first “do no harm”. Most things can be fixed, or at the very least improved upon but the tough cases often require deep wells of knowledge and experience. Sometimes we have to tread into uncharged waters, we just have to make sure we do no harm and try to work around a framework of science based knowledge.
We talk about this concept and video in greater depth in Podcast 90. Feel free to listen in,
here is that link
.
Dr, Shawn Allen
… . just two guys trying to provide logic to things we do not have complete answers for at this time.
For your reading pleasure, here is another fella who has gone through some similar internal dialogue trying to find answers regarding this Voodoo band stuff. We respect his thoughts and dialogue, very much so. He covers many thoughts and theories, it is worth your time if you are using this type of therapy.
http://valeohealthclinic.com/voodoo-floss-really-voodoo/