The Cheetah man: A new perspective on Cross Crawl and neurologic patterning.
A few months ago we wrote a piece about Uner Tan Syndrome. Here was a key point from that blog post (blog post link) and it links beautifully to our most recent controversial blog post on the “Bird Dog” rehab exercise (link here):
[In the video presented in that blog post, and in our “Bird Dog” post photo] there is ipsilateral interference between the foot and hand in this quadrupedal gait. In this diagonal quadrupedal locomotion (QL) the forward moving lower limb is impaired from further forward progression by the posting up (contact) hand of the same side. This would not occur if the QL gait was non-diagonal (ie. unilateral), the forward progression of the lower limb would be met with same time forward progression of the upper limb, allowing a larger striding out of both limbs. This would enable faster locomotion without increasing cadence (which would be the only way of speeding up in the diagonal QL), at the possible limitation of necessitating greater unilateral truncal postural control (which is a typical problem in some of these Uner Tan Syndrome individuals who typically have profound truncal ataxia).
So, why are we showing you the video above today ? If you do not know, go read those 2 blog posts again and look more closely at the video above. At exactly 0:21 seconds into the video, at the slow motion section, you can see what we were talking about in the Bird Dog post last week, that being that the quadrupedal pattern that is neurologically substantiated is that when the right lower limb is in flexion, so is the left upper limb. (we will show these 2 photos in tomorrows post). Where as, “Bird Dog” shows the opposite, that the contralateral upper limb will be in the opposite phase of the contralateral lower limb.
Who cares right ? Well, it matters. In the video above, this could be a problem because if the right leg is in flexion that means that the right arm will be moving into extension. This means that the knee and the hand will be running into each other (look at the baby photo here). As we discussed in the Uner Tan article this will impair faster quadrupedal locomotion. It is also one of the theories as to what may have pushed us to become bipedal and allow faster ambulation (there are many theories of course). So, how then does this guy in the video move like a cheetah ? How is he going so fast with the quadrupedal pattern we have clearly outlined here ?
Within days a blog reader (Micheal L, thanks Michael) messaged us and said this:
-
As a person who likes what’s going on at MoveNat, this type of quadrupedal movement is referred to by them as contralateral movement and is how they teach people to crawl at their seminars. In CrossFit workouts, we also do bear crawls as an exercise, and I always try to maintain a contralateral gait. i.e. Right arm moves forward as left foot comes forwards and vice versa.
So, in other words, in the Uner Tan Syndrome (UTS) the gait is cumbersome and inefficient. In the video above and at MoveNat seminars, it’s a technique/skill.
Did you guys intend for this comparison, or am I out in the cornfield on this?Here was Dr. Uner Tan himself chiming in on the dialogue: -
Üner Tan It is not the same type of locomotion, i.e., not “the diagonal-sequence quadrupedal locomotion”, which is also used by non-human primates.. .Michael: The guy runs so fast it’s hard for me to see it well. Okay, so with UTS the lower limb runs into the upper limb. In this video, his upper limb quickly gets out of the way, giving room for the lower limb (to further flex forward increasing swing phase forward step length). It’s just really hard to see it without slow motion. Thank you for clarifying.
As we said in last weeks post on all of this:
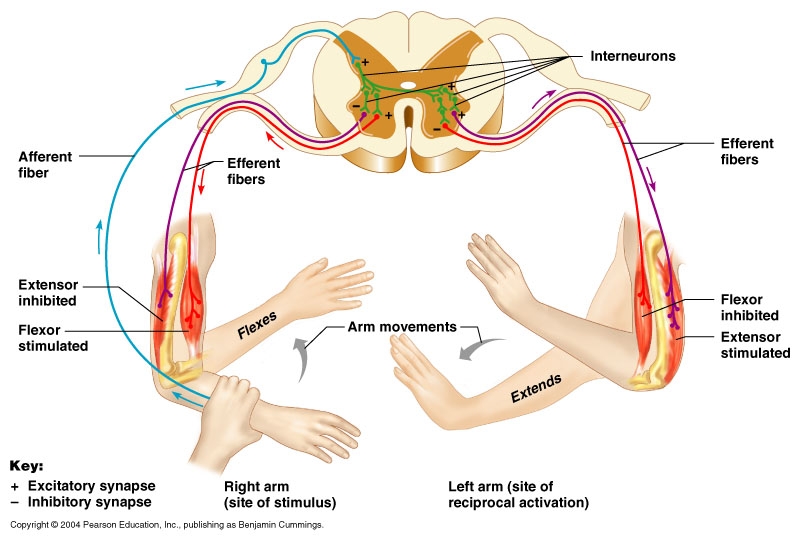
If you look at it neurologically, it is a crossed extensor reflex. It is very similar to a protective reflex called the “flexor reflex” or “flexor reflex afferent”.