We have recently run across some research that has changed the way we look at some of the rehab we do, especially proprioceptive rehab. Perhaps it will do the same for you.
Traditionally, we present increasing balance requirements to the weight bearing structure by changing one or more of the three parameters that keep us upright in the gravitational plane: vision, the proprioceptive system (which include the muscles, joints and ligaments) and the vestibular system (the utricle, saccule and semicircular canals). We have discussed them extensively in multiple articles here on the blog. We generally would make the rehab task more difficult by removing a stimulus (closing your eyes, having someone stand on foam) or challenging (standing on one leg, putting someone on a wobble board, BOSU, extending the head, etc) the to make it more durable and "educated". More difficult task + better balance = more stable joint and better outcomes.
The importaat thing is to think about how much of each system is apportioned; we often (wrongly) assume it is pretty equally divided between the three. It turns out, that it really depends on the surface you are standing on and the circumstances.
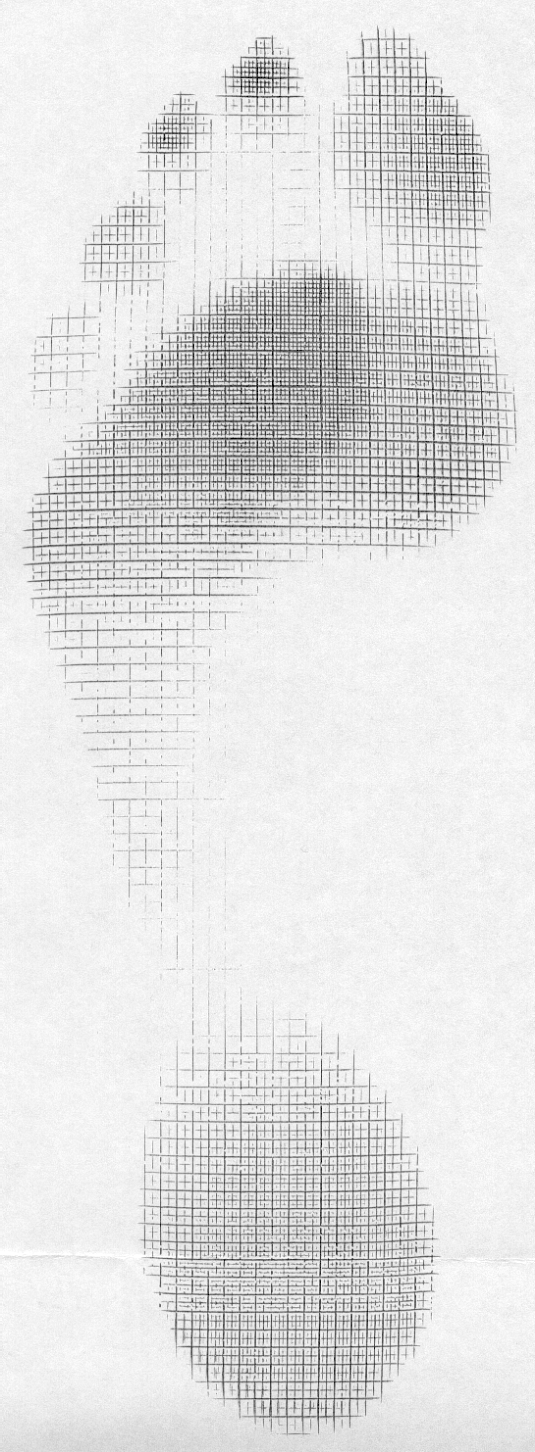
On flat planar surfaces, the division of labor looks something like this:
- proprioceptive system 70%
- vestibular system 20%
- visual system 10 %
On uneven or unstable surfaces (like a BOSU, dynadisc, foam, Swiss ball, etc), it looks like this:
- vestibular system 70%
- visual system 20%
- proprioceptive system 10%
So, if we are rehabbing an ankle, it would make the most sense to do most of the rehab (and additional challenges) on a flat planar surface, perhaps incorporating things like forward, backward and side lean, toe and heel work and closed chain strengthening. WE could also close the eyes to make them more dependent on the proprio system, or extend the head 60 degrees to dampen the influence the lateral semicircular canals. We can put them on a BOSU or unstable surface but we need to remember that in that case, we will be rehabbing the vestibular system AND PERHAPS teaching THAT SYSTEM to compensate more, than the "broken" system. Yes, they get better BUT we are not fixing the system that is injured.
You could make the argument, that your athletes/clients run/walk/exercise on uneven surfaces and use their vestibular system more.Maybe so, but is the actual injury to the vestibular system or to the musculoskeletal one?
Armed with this information, try and think of the system that is compromised and focus your efforts on that system, rather than the other two. Yes, people have vestibular dysfunction and refractive errors and need therapy, exercises and/or corrective lenses, but many of us are not vestibular or opticokinetic therapists (kudos to those of you who are!)
Peterka RJ, Statler KD, Wrisley DM, Horak FB. Postural Compensation for Unilateral Vestibular Loss. Frontiers in Neurology. 2011;2:57. doi:10.3389/fneur.2011.00057.
Horak FB. Postural Compensation for Vestibular Loss. Restorative neurology and neuroscience. 2010;28(1):57-68. doi:10.3233/RNN-2010-0515.