The Latissimus in Gait
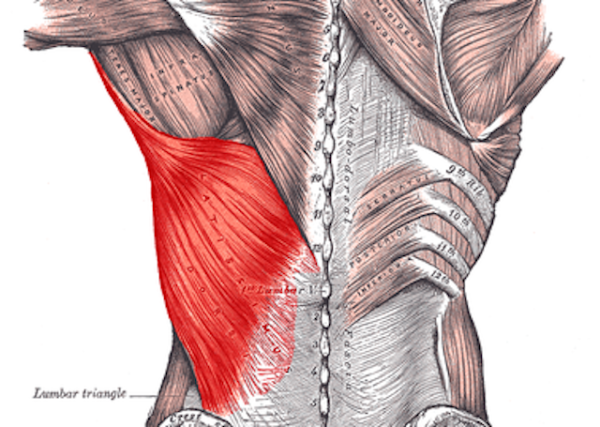
/Affording itself a large attachment centrally from the T7 to L5 spinouses, laterally to the iliac crest and thoracolumbar fascia, rostrally to the lower 3 or 4 ribs and inferior angle of the scapula, to travel superiorly and laterally to the attach to the medial lip of the intertubercular sulcus, it is perfectly situated to effect both the upper and lower extremities in a large variety of movements.
It is one of the quintessential and often overlooked muscles in gait. It is generally quiet electrophysiologically during walking gait (1,2) until speed increases or you are running (2-4). The latissimus dorsi is THE functional link between the upper and lower extremity, particularly though its connections with the thoracolumbar fascia (5,6). Latissimus activity, through gait and arm swing seems to profoundly influence and be influenced by gluteal activity, through the posterior oblique sling system (3,4), consisting of the latissimus dorsi, thoracolumbar fascia and contralateral gluteus maximus (7). The posterior oblique sling system provides trunk stability and power delivery to the upper extremity from the contralateral lower extremity and promotes mutual gait patterns between the upper and lower extremities (8), while creating joint contraction in running, turning and walking (9,10). Recent studies conversely show that arm swing can, in turn, effect lower extremity movement as well (3,4).
Given the importance of the latissimus, it would stand to reason we would want it to function at its best. Dry needling is one modality we seem to be able to use to change its function,not only reducing central sensitization, but reducing local and referred pain, improves range of motion and muscle activation patterns (11-13). There are other modalities, including supportive exercises, that can be used to both activate and rehabilitate the lat as well (14-17)
Here is one method we like to use to needle the latissimus dorsi. Consider adding this to your clinical toolbag.
references:
1. Houglum P, Bertoti D in: Brunstrums Clinical Kinesiology 6th Edition, FA Davis 2012 p.558
2. G. Cappellini, Y. P. Ivanenko, R. E. Poppele, F. Lacquaniti Motor Patterns in Human Walking and Running Journal of Neurophysiology Published 1 June 2006 Vol. 95 no. 6, 3426-3437 DOI: 10.1152/jn.00081.2006
3. Shin S, Kim T, Yoo W. Effects of Various Gait Speeds on the Latissimus Dorsi and Gluteus Maximus Muscles Associated with the Posterior Oblique Sling System. Journal of Physical Therapy Science. 2013;25(11):1391-1392. doi:10.1589/jpts.25.1391.
4. Kim T, Yoo W, An D, Oh J, Shin S. The Effects of Different Gait Speeds and Lower Arm Weight on the Activities of the Latissimus Dorsi, Gluteus Medius, and Gluteus Maximus Muscles. Journal of Physical Therapy Science. 2013;25(11):1483-1484. doi:10.1589/jpts.25.1483.
5. Vleeming A, Pool-Goudzwaard AL, Stoeckart R, van Wingerden JP, Snijders CJ. The posterior layer of the thoracolumbar fascia. Its function in load transfer from spine to legs. Spine (Phila Pa 1976). 1995 Apr 1;20(7):753-8.
6. Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R. The thoracolumbar fascia:anatomy, function and clinical considerations. Journal of Anatomy. 2012;221(6):507-536.doi:10.1111/j.1469-7580.2012.01511.x.
7. Mooney V, Pozos R, Vleeming A, Gulick J, Swenski D Exercise treatment for sacroiliac pain. Orthopedics. 2001 Jan; 24(1):29-32.
8. Page P, Frank C, Lardner R: Assessment and treatment of muscle imbalance. Champaign: Human Kinetics Pub, 2010, pp 30–37.
9. Bergmark A Stability of the lumbar spine. A study in mechanical engineering. Acta Orthop Scand Suppl. 1989; 230():1-54.
10. Collins SH, Adamczyk PG, Ferris DP, Kuo AD A simple method for calibrating force plates and force treadmills using an instrumented pole. Gait Posture. 2009 Jan; 29(1):59-64.
11. Dar G, Hicks GE. The immediate effect of dry needling on multifidus muscles function in healthy individuals. J Back Musculoskelet Rehabil. 2016 Apr 27;29(2):273-278.
12. Ortega-Cebrian S, Luchini N, Whiteley R. Dry needling: Effects on activation and passive mechanical properties of the quadriceps, pain and range during late stage rehabilitation of ACL reconstructed patients.Phys Ther Sport. 2016 Sep;21:57-62. doi: 10.1016/j.ptsp.2016.02.001. Epub 2016 Feb 24.
13. Dommerholt J. Dry needling — peripheral and central considerations. The Journal of Manual & Manipulative Therapy. 2011;19(4):223-227. doi:10.1179/106698111X13129729552065.
14. Youdas JW, Coleman KC, Holstad EE, Long SD, Veldkamp NL, Hollman JH. Magnitudes of muscle activation of spine stabilizers in healthy adults during prone on elbow planking exercises with and without a fitness ball. Physiother Theory Pract. 2017 Sep 18:1-11. doi: 10.1080/09593985.2017.1377792. [Epub ahead of print]
15. Crane P, Ladden J, Monica D. Treatment of axillary web syndrome using instrument assisted soft tissue mobilization and thoracic manipulation for associated thoracic rotation dysfunction: A case report. Physiother Theory Pract. 2017 Aug 30:1-5. doi: 10.1080/09593985.2017.1368755. [Epub ahead of print]
16. Massé-Alarie H, Beaulieu LD, Preuss R, Schneider C. Influence of paravertebral muscles training on brain plasticity and postural control in chronic low backpain. Scand J Pain. 2016 Jul;12:74-83. doi: 10.1016/j.sjpain.2016.03.005. Epub 2016 May 11.
17. Snarr RL, Hallmark AV, Casey JC, Esco MR. Electromyographical Comparison of a Traditional, Suspension Device, and Towel Pull-Up. J Hum Kinet. 2017 Aug 1;58:5-13. doi: 10.1515/hukin-2017-0068. eCollection 2017 Sep.