Change the foot, change the knee (and vice versa). A video case of External Tibial Torsion.
Here is a perfect example of external tibial torsion. Are you treating and training people and messing with their orthotics, squat knee-foot posturing or making gait/running/jumping changes or recommendations? If you are doing all of this and you do not know about tibial torsions, then shame on you, go apologize to these people right now. You could be causing them mechanical grief. Go buy them ice cream (even if they are “paleo”), that fixes most unintentional human mistakes.
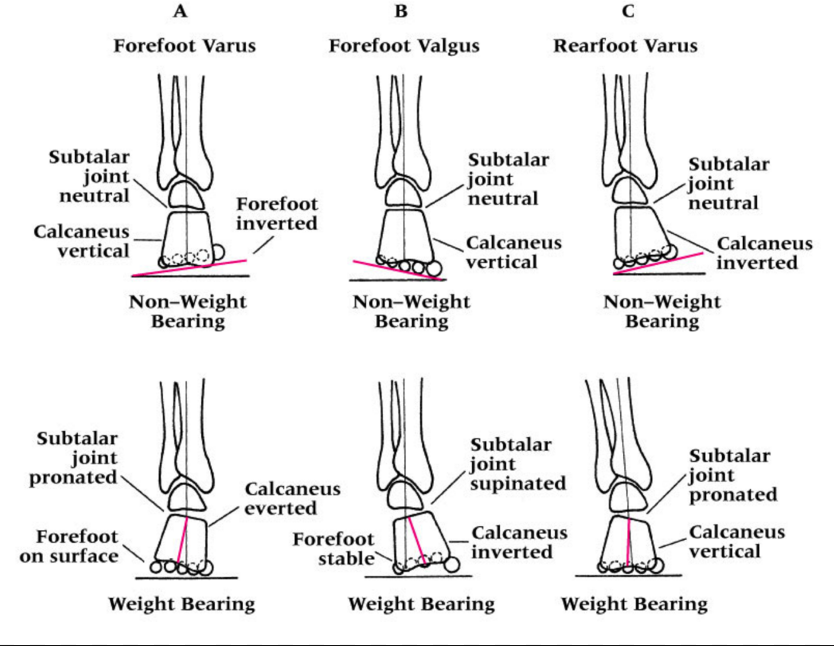
This is a classic presentation of external tibial torsion. This is an anatomic problem, you cannot fix this intrinsically, but you can help extrinsically. You teach these people about this issue and why the foot and the knee cannot cooperate. You teach them why their feet are spun out (increased foot progression angle) while their knee tracks straight forward sagittally. You teach them why they might heel strike far laterally and why their pronation phase might be abrupt. As in this video, you teach them why they might fashionably choose to narrow the foot progression angle (foot turned in) while at the same time having to bear weight on the lateral foot (in supination to externally spin the tibia) to keep the knee tracking sagittally. You teach them why this will be impossible to do in pumps (inversion sprain ouch) and why over time this will anger many joints and tendons. You teach them that without this accommodation they will track the knee inside the sagittal plane (as seen in the video). You teach them why they might be at greater risk of having foot prontation issue pathologies, why they might have limited internal hip rotation, why orthotics likely do not do much for them (yes, there are exceptions), why certain shoes are a challenge for them while others are magical and why over time their once beautiful arch has begun to “fall” and be less prominent as they attenuate the plantar tissues.
As you get good with this gait and biomechanics stuff, you should readily see and understand all of the issues discussed here today in a mere flash of instant brilliance so you know what to offer your client, in understanding and remedy options. As you have seen in this video, when left to their own devices, they naturally allow the knee to find the sagittal plane in a nice forward hinge. In this posture the foot is excessively progressed outward. Again, this is because of the tibial long bone torsion. This is their anatomy, this is not functional in this case. You cannot fix this, you help them manage this, first with their awareness, then with your brilliance. You may implement exercises and gait strategies to help them become aware of mechanical issues and how to protect the foot-ankle, the knee and the hip. You teach them why they might have a tendency towards anterior pelvis posturing or sway back type postures. You teach them why, in some cases, they choose knee hyperextension as a comfortable yet lazy stance postural habit. You teach them why some shoes are “happy” shoes for them, and why others are pure evil.
A foundational principle we teach here at The Gait Guys is that the knee is a simple hinge between two multiaxial joints on either side of the knee, the hip and the foot-ankle complex. The knee really can only flex and extend, and when the mechanics above and below are challenged the knee has little depth to its abilities to tolerate much of anything except simple sagittal hinging. You can see that the foot posturing and tibial torsion rule the roost here in this video. You should learn in time that managing this case above and below the knee is where the pot of gold is found. You will learn in time that taping the knee is often futile, yet a worthy experiment both for you and the client in the discovery process, but that a life time of taping is not logical. External tibial torsion, although affording the knee that sagittal hinge plane, can narrow its range of safe sagittal mechanics and it is up to you to help them learn and discover that razor’s edge safely and effectively when the torsion is large. You should also discuss with them that as they plastically tissue adapt over the years (ie. pronate more and lose more arch integrity), this razor’s edge may widen or narrow for the knee mechanics as well as the hip and foot-ankle complex.
For your reading pleasure, a classic example of how to interrogate a safe sagittal knee progression was discussed in this blog video piece we wrote recently, linked here.
Look and you shall find, but only if you know what you are looking for.
* Please now know that you should never off the cuff tell someone to turn inwards their outwardly spun foot. But if you do, have ice cream on hand, just in case.
Need more to spin your head ? Think about whether their IT band complex is going to be functioning normally. Oy, where is that ice cream !
Shawn Allen, one of the gait guys