In searching our personal archives for neat stuff we came across an oldie but a goodie. One to certainly make your head spin. We do not even know where this came from and how much was our original material and how much was someone else’s. If you can find the reference we would love to give it credit. We do now that we added some stuff to this but we don’t even know what parts were ours ! Regardless, there is a brain twister here worth juggling in your heads. Lets start with this thought……..
When you are sitting the rectus femoris (a quad muscle) is “theoretically” shortened because the hip is in flexion. It crosses the bent knee in the front at it blends with the patellar tendon, thus it is “theoretically” lengthened at the knee. When we stand up, the hip extends and the knee extends, making the R. Femoris “theoretically” lengthen at the hip and shorten at the knee. This, it bodes the question…….did the R. Femoris even change length at all ? And the hamstrings kind of go through the same phenomenon. It is part of the uniqueness of “two joint” muscles. Now, onto Lombard’s paradox with more in depth thought on this topic.
Warren Plimpton Lombard (1855-1939) sought to explain why the quadriceps and hamstring muscles contracted simultaneously during the sit-to-stand motion. He noted that the rectus femoris and the hamstrings are antagonistic, and this coactivation is known as Lombard’s paradox.
The paradox is classically explained by noting the relative moment arms of the hamstrings and rectus femoris at either the hip or the knee, and their effects on the magnitude of the moments produced by either muscle group at each of the two joints.
By virtue of the fact that muscles cannot develop different amounts of force in their different parts, the paradox develops. The hamstrings cannot selectively extend the hip without imparting an equal force at the knee. Thus, the only way for hip extension and knee extension to occur simultaneously in the act of standing (or eccentrically in the act of sitting) is for the net moment to be an extensor moment at both the hip and knee joints. Lombard suggested three necessary conditions for such paradoxical co-contraction:
- the lever arm of the muscle must be greater at its extensor end
- a two-joint muscle must exist with opposite function
- the muscle must have sufficient leverage so as to use the passive tendon properties of the other muscle
In 1989, Felix Zajac & co-workers pointed out that the role of muscles, particularly two-joint muscles, was much more complex than has traditionally been assumed. For example, in certain situations, the gastrocnemius could act as a knee extensor. It is clear now that the direction in which a joint is accelerated depends on the dynamic state of all body segments, making it difficult to predict the effect of an individual muscle contraction without extensive and accurate biomechanical models (Zajac et al, 2003).
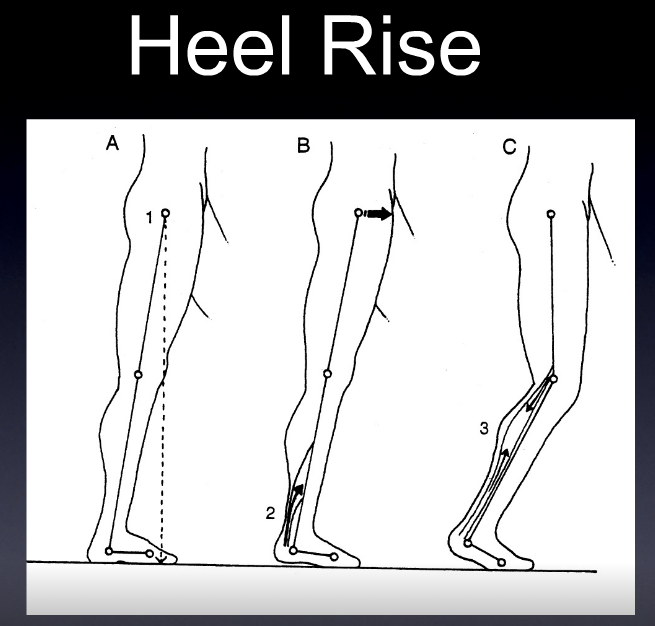
In fact, back to the gastrocnemius another 2+ joint muscle (crosses knee, mortise and subtalar joints), we all typically think of it as a “push off” muscle. It causes the heel to rise and accelerates push off in gait and running. But, when the foot is fixed on the ground the insertion is more stable and thus the contraction, because the origin is above the posterior joint line, can pull the femoral condyles into a posterior shear vector. It thus, like the hamstrings, needs to be adequately trained in a ACL or post-operative ACL, deficient knee to help reduce the anterior shear of normal joint loading. It is vital to note, that when ankle rocker is less than 90 degrees (less than 90 degrees of ankle dorsiflexion is available), knee hyperextension is a viable strategy to progress forward in the sagittal plane. But in this scenarios, the posterior shear capabilites of the gastrocnemius are brought to the front of the line as a frequent strategy. And not a good one for the menisci we should mention.
Andrews J G (1982) On the relationship between resultant joint torques and muscular activity Med Sci Sports Exerc 14: 361-367.
Andrews J G (1985) A general method for determining the functional role of a muscle J Biomech Eng 107: 348-353.
Bobbert MF, van Soest AJ (2000) Two-joint muscles offer the solution - but what was the problem? Motor Control 4: 48-52 & 97-116.
Gregor, R.J., Cavanagh, P.R., & LaFortune, M. (1985). Knee flexor moments during propulsion in cycling–a creative solution to Lombard’s Paradox. Journal of Biomechanics, 18, 307-16 .
Ingen-Schenau GJv (1989) From rotation to translation: constraints on multi-joint movement and the unique action of bi-articular muscles. Hum. Mov. Sci. 8:301-37.
Lombard, W.P., & Abbott, F.M. (1907). The mechanical effects produced by the contraction of individual muscles of the thigh of the frog. American Journal of Physiology, 20, 1-60.
Mansour J M & Pereira J M (1987) Quantitative functional anatomy of the lower limb with application to human gait J Biomech 20: 51-58.
Park S, Krebs DE, Mann RW (1999) Hip muscle co-contraction: evidence from concurrent in vivo pressure measurement and force estimation. Gait & Posture 10: 211-222.
Rasch, P.J., & Burke, R.K. (1978). Kinesiology and applied anatomy. (6th ed.). Philadelphia: Lea & Febiger.
Visser JJ, Hoogkamer JE, Bobbert MF & Huijing PA (1990) Length and Moment Arm of Human Leg Muscles as a Function of Knee and Hip Angles. Eur. J Appl Physiol 61: 453-460.
Zajac FE & Gordon MF (1989) Determining muscle’s force and action in multi-articular movement Exerc Sport Sci Revs 17: 187-230.
Zajac FE, Neptune RR, Kautz SA (2003) Biomechanics and muscle coordination of human walking - Part II: Lessons from
dynamical simulations and clinical implications, Gait & Posure 17 (1): 1-17.