This is a nice study looking at lateral gastroc activity and changing firing patterns with speed of movement. Great if you treat anyone or anything that walks...
Ia afferents
You remember them, large diameter afferent (sensory) fibers coming from muscle spindles and appraising the nervous system of vital information like length and rate of change of length of muscle fibers, so we can be coordinated. They act like volume controls for muscle sensitivity. Turn them up and the muscle becomes more sensitive to ANY input, especially stretch (so they become touchy…maybe like you get if you are hungry and tired and someone asks you to do something); turn them down and they become less or unresponsive.
Their excitability is governed by the sum total (excitatory and inhibitory) of all neurons (like interneuron’s) acting on them (their cell bodies reside in the anterior horn of the spinal cord).
If we slow things down, the rate of change of length slows as well and excitability decreases, like we see in this study (3-6% slower). We also notice that the length of contraction increases; hmmm, why doesn’t it decrease?
Remember these folks are on a treadmill. The treadmill is constantly moving, opposite the direction of travel. With the foot on the ground, this provides a constant rate of change of length of the gastroc/soleus (ie, it is putting it through a slow stretch); so , once the muscle is activated, it contracts for a longer period of time because of the treadmill putting a slow stretch on the gastroc (and soleus).
This article also talks about people with upper motor neuron lesions. An important set of inhibitory neurons come from higher centers of the brain, in the motor cortex. These tend to attenuate the signals affecting the Ia afferents, and keep us stable. When we have an upper motor neuron lesion (like a brain lesion or stroke), we lose this “attenuation” and the stretch reflexes (and muscle tone) becomes much more active (actually hyperactive), making the muscle more sensitive to stretch. This loss of attenuation, along with differing firing patterns of the gastroc are important to remember in gait rehab.
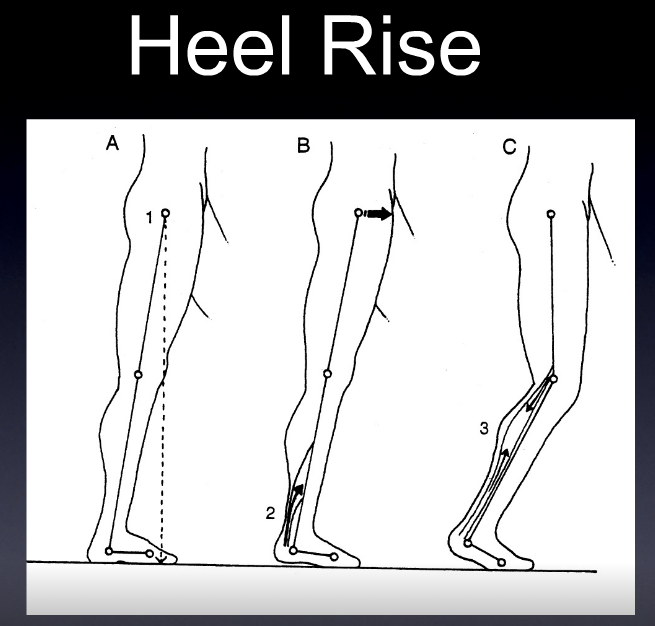
The soleus and medial gastroc begin firing in the first 10% of the gait cycle (at the beginning of loading response) and fire continuously until pre swing (peaking just after midstance). The lateral head begins firing at midstance; both heads (along with soleus) decelerate the forward momentum of the tibia, flex the knee at midstance, and the medial head assists in adducting the calcaneus to assist in supination.
Making sure these muscles fire appropriately is important and needling is just one way of helping them to function better. Don’t overlook the tricep surae on your next patient that has a “hitch in their giddyup”.
Effects of treadmill walking speed on lateral gastrocnemius muscle firing.
by Edward A Clancy, Kevin D Cairns, Patrick O Riley, Melvin Meister, D Casey Kerrigan
American journal of physical medicine rehabilitation Association of Academic Physiatrists (2004) Volume: 83, Issue: 7, Pages: 507-51 PubMed: 15213474
Abstract
OBJECTIVE: To study the electromyographic profile-including ON, OFF, and peak timing locations-of the lateral gastrocnemius muscle over a wide range of walking speeds (0.5-2.1 m/sec) in healthy young adults. DESIGN: We studied gastrocnemius muscle-firing patterns using an electromyographic surface electrode in 15 healthy subjects ambulating on a treadmill at their normal walking speed and at three paced walking speeds (0.5, 1.8, and 2.1 m/sec). Initial heel contact was determined from a force-sensitive switch secured to the skin over the calcaneous. RESULTS: For all speeds, the gastrocnemius firing pattern was characterized by a main peak, occurring 40-45% into the gait cycle, that increased in amplitude with walking speed. Speeds of > or =1.3 m/sec produced a common electromyographic timing profile, when the profile is expressed relative to the stride duration. However, at 0.5 m/sec (a speed typical of individuals with upper-motor neuron lesions), the onset of gastrocnemius firing was significantly delayed by 3-6% of the gait cycle and was prolonged by 8-11% of the gait cycle. CONCLUSION: Many patients with upper motor neuron lesions (e.g., stroke and traumatic brain injury) walk at speeds much slower than those commonly described in the literature for normal gait. At the slow walking speed of 0.5 m/sec, we have measured noticeable changes in the electromyographic timing profile of the gastrocnemius muscle. Given the importance of appropriate plantar flexor firing patterns to maximize walking efficiency, understanding the speed-related changes in gastrocnemius firing patterns may be essential to gait restoration.