The tibialis posterior (TP) is one of the more important extrinsic arch stabilizing muscles. It is a stance phase muscle that fires from the loading response through terminal stance, acts eccentrically to loading response to mid stance to slow pronation and concentrically from mid stance to terminal stance to assist in supination.(4) Its recruitment seems to be increased with slower walking speeds (5).
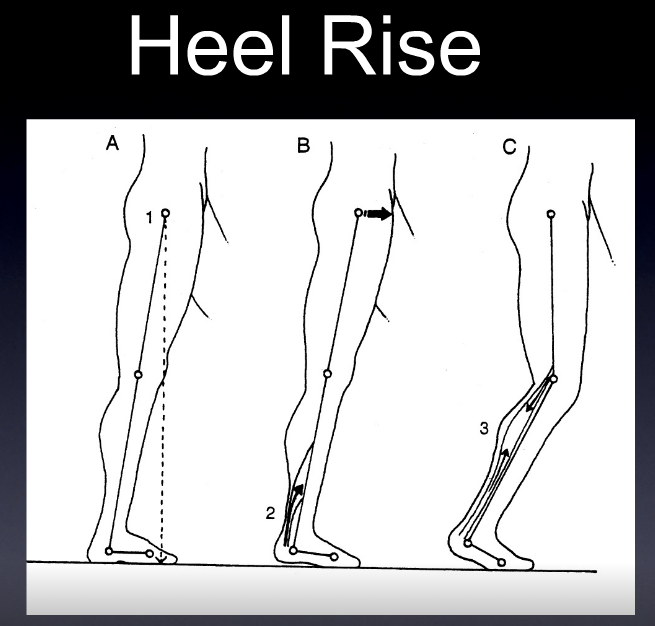
Since the foot is usually planted when it fires, we must look at its closed chain function (how it functions when the foot/insertion is fixed on the ground), which is predominantly maintenance of the medial longitudinal arch, with minor contributions to the transverse metatarsal and lateral longitudinal arches (6) ; flexion and adduction of the tarsal’s and metatarsals and eccentric slowing of anterior translation of the tibia during ankle rocker. It is also an external rotator of the lower leg and is the prime muscle which decelerates internal rotation of the tibia and pronation. As the origin and insertion are concentrically brought towards each other during early passive heel lift it becomes a powerful plantarflexor and inverter of the rearfoot. There is also a component of ankle stabilization via posterior compression of the tarsal’s and adduction of the tibia and fibula.
Alas, there is much more than the typical open chain functions of plantar flexion, adduction and inversion. Perhaps it is some of these other, closed chain functions, that cause the “progressive nature of posterior tibial tendon dysfunction"(7)?
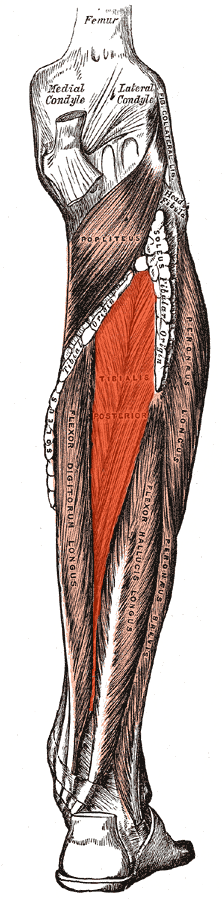
This muscle is easily accessed through the posterior compartment, lying deep in the midline to the gastroc and soleus (8,9). Care should be taken to avoid the sural nerve, often found between the heads of the gastroc and becoming superficial (and palpable) in the midline where it exits from the inferior junction of the 2 heads of the gastroc (10). The posterior tibial artery, vein and nerve lie on top of the tibialis posterior for the upper 2/3 of its route through the calf, becoming superficial (and palpable) in the distal 1/3 of the lower leg (11). I find starting laterally or medially and angling your fingers, instrument or the needle medially or laterally seems to work best. Make sure to count your layers!
1. Ling SK, Lui TH. Posterior Tibial Tendon Dysfunction: An Overview. Open Orthop J. 2017 Jul 31;11:714-723. doi: 10.2174/1874325001711010714. eCollection 2017. link to free full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5620404/
2. Blake R.L., Anderson K., Ferguson H. Posterior tibial tendinitis. A literature review with case reports. J. Am. Podiatr. Med. Assoc. 1994;84(3):141–149. doi: 10.7547/87507315-84-3-141. [PubMed] [Cross Ref]
3. Supple K.M., Hanft J.R., Murphy B.J., Janecki C.J., Kogler G.F. Posterior tibial tendon dysfunction. Semin. Arthritis Rheum. 1992;22(2):106–113. doi: 10.1016/0049-0172(92)90004-W. [PubMed] [Cross Ref]
4. Semple R, Murley GS, Woodburn J, Turner DE. Tibialis posterior in health and disease: a review of structure and function with specific reference to electromyographic studies. Journal of Foot and Ankle Research. 2009;2:24. doi:10.1186/1757-1146-2-24.
link to free full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2739849
5. Murley GS1, Menz HB2, Landorf KB2. Electromyographic patterns of tibialis posterior and related muscles when walking at different speeds. Gait Posture 2014 Apr;39(4):1080-5. doi: 10.1016/j.gaitpost.2014.01.018. Epub 2014 Feb
6. Kaye RA1, Jahss MH. Tibialis posterior: a review of anatomy and biomechanics in relation to support of the medial longitudinal arch. Foot Ankle. 1991 Feb;11(4):244-7.
7. Rabbito M, Pohl MB, Humble N, Ferber R. Biomechanical and Clinical Factors Related to Stage I Posterior Tibial Tendon Dysfunction. J Orthop Sports Phys Ther, Epub 12 July 2011.doi:10.2519/jospt.2011.3545.
8. Howitt S, Jung S, Hammonds N. Conservative treatment of a tibias posterior strain in a novice triathlete: a case report. J Can Chiropr Assoc. 2009 Mar;53(1):23-31. link to free full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2652628/
9. Lou XF, Yang XD, Jiang SH, Sun CY, Zhang RF.[Study on angle and depth of needle insertion in acupuncture at Zusanli (ST 36)]. Zhongguo Zhen Jiu. 2006 Jul;26(7):483-6
10. https://functionalanatomyblog.com/2009/11/26/the-sural-nerve-anatomy-and-entrapment/
11. Enrique Ginzburg, ... Norman M. Rich VASCULAR ANATOMY OF THE EXTREMITIES in Current Therapy of Trauma and Surgical Critical Care, Mosby; Pages 467–472 2008