Beyond the Trigger Point...
Many clinicians needle. We are taught to dry needle trigger points and to needle the segmental innervation of the muscle involved. But should we do more? I think so, and here is one paper on incorporating needling myofascial meridians along with trigger points that supports that notion (1).
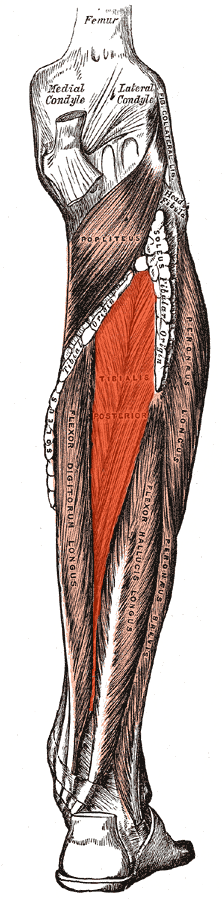
Since most of us treat patients that are ambulatory, we should be thinking of how a patient moves, especially through the gait cycle. Think of the kinetic chain in what I like to call “reverse engineering”, that is, from the ground up, rather from the torso down, in a closed chain fashion. This will profoundly effect the way you look at muscle function, for example: thinking of the vastus lateralis as a medial rotator of the thigh (yes, you read that right; think about it and try and get your head wrapped around it), or of the peroneus longus as an abductor of the lower leg and external rotator (assisting supination) during the latter half of the gait cycle. Reverse engineering gives you a whole new outlook on locomotion and human movement.
Tom Myers was insightful enough to write a great text talking about myofascial meridians or “lines of tissue stress ” describing the fascial connections of muscles utilized in a chain during movement (2). This built upon the original work of Valdimir Janda and his concepts of “loops and slings” (3), as well as the work of Paoletti (4) and Vleeming (5).
In neurology, we have the conjoint concepts of temporal and spacial summation that can lead to some action on the part of the nervous system. They describe 2 ways that receptors or neurons can reach threshold and fire an action potential (6) .
Temporal summation is when a receptor or neuron is stimulated repetetively over time, with each potential bulding upon the previous, making the stimulus effectively larger and larger. If you were in a movie theater and the person seated behind you kept hitting the back of your seat repetitively (temporal summation), it would only be a matter of time before you turned around and said some thing to them(ie, you reached threshold).
Spacial summation is when a receptor or neuron is stimulated at multiple locations over time, with the potentials building and bringing the receptor or neuron closer to threshold. Taking the same scenario as before, if many people began hitting your chair from multiple directions (spacial summation), it would be only a matter of time before you said something (ie: reached threshold).
These two things can work together as well, usually eliciting a result much faster, since the receptor or neuron is being hit multiple times from multiple directions and it can usually reach threshold faster.
Since one of our goals in needling is not only to reduce or eliminate the trigger point, but also to reduce pain and increase function, wouldn’t it make sense to take advantage of as much neurology as possible? How about more real estate (spacial summation) in a reasonable time frame from point to point (temporal summation)?
Needling appears to cause pain modulation, as well as many of its other effects, through both peripheral and central mechanisms (7,8). Having our therapy stimulate more of these mechanisms should theoretically make our therapy more effective and improve outcomes. So, more needles may be a good thing, no?
Getting back to the paper (1), they needled tender points (satellite trigger points?) along the lower portions of the “superficial back line” or “SBL”, along with points on the foot for plantar fascitis. The SBL contains plantar fascia, Achilles tendon, gastrocnemius,hamstrings, sacrotuberous ligament, and erector spinae. It continues to the suboccipital muscles and ends at the suboccipital muscles, galea aponeurotica of the skull and ultimately the frontalis muscle (2). They could have incorporated more, and perhaps had even better results, as the upper cervial spine contains one of the highest densities of mechanoreceptors in the body (9, 10), and afferent information from the upper 4 cervical neuromeres feed directly into the flocculonodular lobe of the cerebellum (11, 12).
So, how about incorporating myofascial meridians into your needling toolbox? The next time you see someone with a problem area, think about the kinetic chain that gets you there, starting from the ground up, and incorporate THAT into your treatment protocol.
references:
1. Akhbari B, Salavati M, Ezzati K, Mohammadi Rad S: The Use of Dry Needling and Myofascial Meridians in a Case of Plantar Fasciitis Journal of Chiropractic Medicine (2014) 13, 43–48
2. Myers TW. Anatomy trains: myofascial meridians for manual and movement therapists. 2nd ed. Philadelphia: Churchill Livingstone; 2009.
3. Janda V, Vavrova M, Hervenova A, et al. Sensory motor stimulation. In: Liebenson C. ed Rehabilitation of the spine: a practitioner’s manual. 2nd edn. Lippincott Williams & Wilkins, 2006.
4. Paoletti S. The fasciae: anatomy, dysfunction & treatment. Eastland Press; 2006.
5. Vleeming A, Snijders C, Stoeckart R, Mens J. The role of the sacroiliac joins in coupling between spine, pelvis, legs and arms. In: Vleeming A, et al, editor. Movement, stability and low back pain. Churchill Livingstone; 1997. p. 53–71
6. Levin & Luders (2000). Comprehensive Clinical Neurophysiology. New York: W.B. Saunders Company.
7. Dommerholt j Dry needling — peripheral and central considerations Journal of Manual and Manipulative Therapy 2011 VOL. 19 NO. 4 223-237
8. Li-Wei Chou, Mu-Jung Kao, Jaung-Geng Lin ProbableMechanisms of Needling Therapies for Myofascial Pain Control Evidence-Based Complementary and Alternative Medicine Volume 2012, Article ID 705327, 11 pages doi:10.1155/2012/705327
9. Kulkarni V1, Chandy MJ, Babu KS Quantitative study of muscle spindles in suboccipital muscles of human foetuses. Neurol India. 2001 Dec;49(4):355-9
10. Bogduk N Cervicogenic headache: anatomic basis and pathophysiologic mechanisms. Curr Pain Headache Rep. 2001 Aug;5(4):382-6.
11. Luan H1, Gdowski MJ, Newlands SD, Gdowski GT Convergence of vestibular and neck proprioceptive sensory signals in the cerebellar interpositus. J Neurosci. 2013 Jan 16;33(3):1198-210a. doi: 10.1523/JNEUROSCI.3460-12.2013.
12. Seaman D Winterstein Dysafferentation: A Novel Term to Describe the Neuropathophysiological Effects of Joint Complex Dysfunction. A Look at Likely Mechanisms of Symptom Generation J Manipulative Physiol Ther 1998 (May); 21 (4): 267-280