The Truth About Treadmills: A Neurological Perspective
Gender differences in walking and running on level and inclined surfaces.
Chumanov ES, Wall-Scheffler C, Heiderscheit BC. Clin Biomech (Bristol, Avon). 2008 Dec;23(10):1260-8. Epub 2008 Sep 6.
What the Gait Guys have to say about this article:
This article highlights some of the differences in gait between males and females on treadmills. Though treadmills don’t necessarily represent real life, they are an approximation. While reading this article, please keep the following in mind:
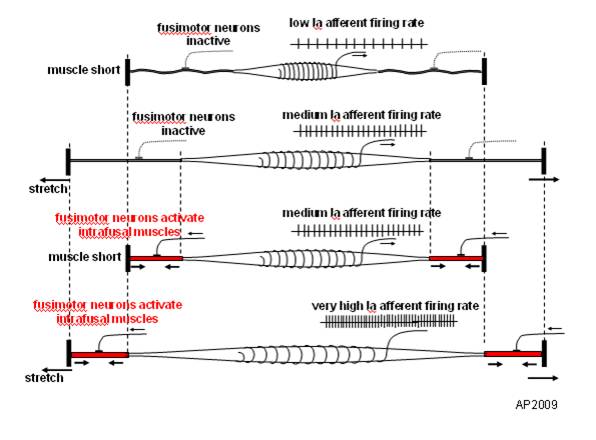
1. the treadmill pulls the hip into extension and places a pull on the anterior hip musculature, especially the hip flexors including the rectus femoris, iliopsoas and iliacus. This causes a slow stretch of the muscle, activating the muscle spindles (Ia afferents) and causing a mm contraction (ie the stretch reflex). This acts to inhibit the posterior compartment of hip extensors (especially the glute max) through reciprocal inhibition, making it difficult to fire them.
2. Because the deck is moving, the knee is brought into extension, with stretch of the hamstrings, the quads become reciprocally inhibited (same mechanism above).
3. The moving deck also has a tendency to put the ankle in dorsiflexion, initiating a stretch reflex in the tricep surae (gastroc/soleus) facilitating toe off through here and pushing you through the gait cycle, rather than pulling you through (with your hip extensors).
4. the moving deck forces you to flex the thigh forward for the next footstrike (ie footstance), firing the RF, IP and Iliacus, and reciprocally inhibit the g max
If your core isn’t engaged, the pull of the rectus femoris and iliopsoas/iliacus pulls the ilia and pelvis into extension (ie increases the lordosis) and you reciprocally inhibit the erectors and increase reliance on the multifidus and rotatores, which have short lever arms and are supposed to be more proprioceptive in function. Can you say back pain?
In summary, treadmills are not the scourge of humanity, but do have some pitfalls for training, and equal amounts of “backwards” running should be employed (with great caution, mind you)
With that being said, lets look at the results: increased hip internal rotation and adduction, as well as more glute activity for the ladies. Not surprising considering women generally have a larger Q angle (17 +/- 3 degrees for females, 14 +/-3 degrees for males) and greater amounts of hip anteversion (average 14 degrees in females vs 8 in males). The larger Q angle places more stress at the medial knee (compression of the medial femoral condyle and usually increased pronation as the center of gravity over the foot is moved medially) and thus more control needed to slow pronation (from the glutes to control/augment internal rotation). Greater hip anteversion means the angle of the femoral head is greater than 12 degrees to the shaft of the femur. This moves the lower extremity into a more internally rotated position, approximating the origin and insertion of the adductors, making them easier to access. With an increased Q angle and easier access, greater demands are placed on adductors in single leg stance (which is considerably greater in running), This increased adductory moment places more demand on the gluteus medius (and contralateral QL) as well, to stabilize the pelvis and this correlates with speed and incline, also found in the study.
The take home message? Don’t throw away your treadmill! The treadmill can be an excellent diagnostic tool! Gluteal and adductor insufficiencies will be more visible (and probably more prevalent) in females, especially those running or walking on treadmills. The hip extension and ankle dorsiflexion moment created by a treadmill works against some of the stabilizing mechanisms (glute inhibition, ankle dorsiflexor inhibition) and help to highlight some of the subtle gait abnormailities you may miss otherwise.
Abstract from Article
BACKGROUND: Gender differences in kinematics during running have been speculated to be a contributing factor to the lower extremity injury rate disparity between men and women. Specifically, increased non-sagittal motion of the pelvis and hip has been implicated; however it is not known if this difference exists under a variety of locomotion conditions. The purpose of this study was to characterize gender differences in gait kinematics and muscle activities as a function of speed and surface incline and to determine if lower extremity anthropometrics contribute to these differences.
METHODS: Whole body kinematics of 34 healthy volunteers were recorded along with electromyography of muscles on the right lower limb while each subject walked at 1.2, 1.5, and 1.8m/s and ran at 1.8, 2.7, and 3.6m/s with surface inclinations of 0%, 10%, and 15% grade. Joint angles and muscle activities were compared between genders across each speed-incline condition. Pelvis and lower extremity segment lengths were also measured and compared.
FINDINGS: Females displayed greater peak hip internal rotation and adduction, as well as gluteus maximus activity for all conditions. Significant interactions (speed-gender, incline-gender) were present for the gluteus medius and vastus lateralis. Hip adduction during walking was moderately correlated to the ratio of bi-trochanteric width to leg length.
INTERPRETATION: Our findings indicate females display greater non-sagittal motion. Future studies are needed to better define the relationship of these differences to injury risk.
PMID: 18774631 [PubMed - indexed for MEDLINE]
Yup, we’re gait nerds….Don’t laugh….You are too if you are reading this…..
The Gait Guys: finding other uses for treadmills, other than for hanging the laundry…..