Zonas vs K Tape
/image source: https://commons.wikimedia.org/wiki/File:Kinesio_Taping_for_Soleus_and_Achilles_tendon.jpg
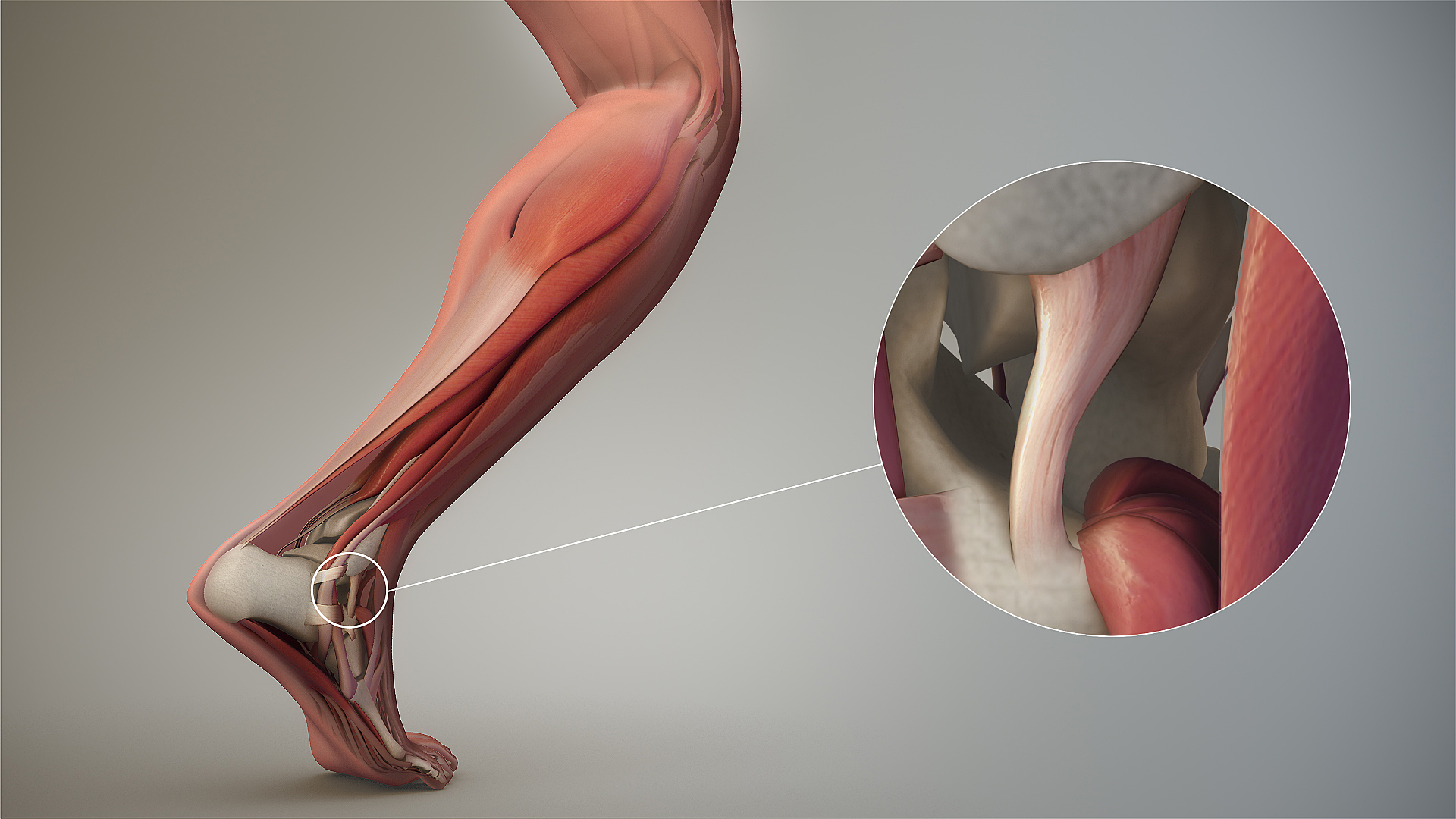
In this case, flexibility and an elastic component (K Tape), which adds proprioception, rather than rigid (Zonas), which takes it away, seems to work better.
"Compared to Athletic Tape, Kinesio Tape (KT) provides a flexible pulling force that facilitates foot eversion during early stance, while not restricting normal inversion in late stance during walking. KT may be a useful clinical tool in correcting aberrant motion while not limiting natural movement in sports."
Yen SC, Folmar E, Friend KA, Wang YC, Chui KK. Effects of kinesiotaping and athletic taping on ankle kinematics during walking in individuals with chronic ankle instability: A pilot study. Gait Posture. 2018 Aug 28;66:118-123. doi: 10.1016/j.gaitpost.2018.08.034. [Epub ahead of print]