We have an interesting gait video case for you today. All we can say is, watch it through the end for the great finale !
Here is the link:
http://youtu.be/7lXS_JzxTAY
Sleep Leads to Performance.
/Here is a piece Dr. Allen contributed to for www.superhumancoach.com and for Competitor.
http://www.superhumancoach.com/2012/sleep-leads-to-performance/
Dr. Shawn Allen, of “The Gait Guys” and ACO, treats many high level athletes. “[He] finds that two things are commonly abused when it comes to effective training, recovery and sleep. Many athletes overtrain and ignore the restorative benefits of ample recovery days but of the two, sleep is the most abused. In this day and age of productivity in the work place and family demands the average athlete has little time to train, work and recover adequately. And since work and family demands are less flexible, sleep for many tends to take a back seat.” Dr. Allen explains that there is no nutritional supplement or drug that can replace the benefits of a sound night sleep. “And yet, we continue to do what we need to do to get our workouts in, a valid yet jaundiced attempt to benefit our bodies, while at the same time sacrificing the beneficial aspects of health and recovery that can come only with sound repeatable sleep”.
leg length discrepancies and shoe lifts
/Leg length discrepancies (LLD’s) are encountered on a daily basis. They are the root of many ankle, knee, hip and spinal problems. The questions the clinician must ask are “How much is significant?”, “How much do I add?” What are some of the signs and symptoms?” “What is the etiology?” and “How do I detect it?” A literature search (2003) provided the following information and answers.
How much is significant?
Most authorities claim that deficiencies of greater than ¼ inch (6mm) are clinically significant (1, 2) though some sources state that differences as little as 4 mm are significant (5). Subotnick (3) states that because of the threefold increase in ground reactive forces with running, lifts should be used with inequalities of greater than 1/8” inch (3mm).
How much do I add?
One of the easiest ways to determine the amount of lift needed is to examine the person in a weight bearing posture and add lifts under the short leg until the pelvis is even or until the lumbar spine is straight. If using off weight bearing measurements, you need to add 1/3 more height than measured because the talus is positioned 1/3 of the way between the calcaneus and metatarsal heads (4, 13). So, a heel lift placed under the calcaneus will only raise the talus 2/3 of that height. Lifts placed under the calcaneus can shorten the tricep surae muscles (4, 6) and apply increased pressure to the metatarsal heads (12); full length sole lifts are more physiological, though not always practical. Due to the supinatory moment of the short leg on heel strike, a lift may cause overcompensation and increased supination, with a tendency to overweight the lateral column and possibly injure the lateral ankle. Careful observation of gait post addition of a lift is in order and a valgus post running at least the length of the 5th metatarsal along with the lift should be considered (8, 9). Heel lifts also cause EMG changes of leg muscles, with decreased recruitment of gastrocnemius and tibialis anterior directly proportional to the height of the heel lift (18, 19). A lift or LLD changes the ground reactive forces associated with gait, increasing vertical force on the longer leg, along with increased joint stresses along the kinetic chain (14, 20).
Generally speaking, lifts greater than 3/8” (9mm) require extrinsic modifications to footwear (4, 6, 8). Find a competent individual to perform this work for you. Large discrepancies should be treated gradually, at a rate of ¼ inch every 4 weeks, less if symptoms do not permit.
What are signs and symptoms associated with LLD’s?
Compensation comes in many forms, depending whether it is acute (recent injury caused an LLD or compensation resulting in one, or long term. The deficiency can cause injury on the short or long legged side (or both).
The long leg moves through a greater arc during all portions of swing phase (7). The person may flex the knee to compensate and shorten the arc. The individual may also maximally pronate and evert the calcaneus an additional 3 degrees or greater on that side in an attempt to lower the navicular to the ground and shorten that leg. This causes an increased amount of internal rotation of the tibia and thigh causing muscular dysfunction (tightness of the hip flexors, strain of the intrinsic external rotators from eccentric deceleration of the thigh), along with medial knee strain (especially with concomitant genu valgus) (4, 6, 8, 9, 10, 11, 21, 22).
The short leg side will often supinate in an attempt to lengthen and cushion some of the shock of heel strike, since it has a greater vertical distance to travel (14); this often occurs with hyperextension of that knee. This lessens the dampening ability of the knee (since it flexes almost 20 degrees between heel strike and full forefoot load), and speeds the rate of subtalar pronation (since the rear foot is inverted and still must pronate the same amount (4). Many individuals will try and attenuate impact by contracting the contralateral hip abductor muscles and eccentrically lower the shorter extremity (4, 14). This can produce excessive strain of that musculature (trochanteric bursitis) as well as pathomechanical abnormalities of the L4 and L5 motion segments (due to increased body rotation toward the short side and attachments of the iliolumbar ligaments; this can cause degenerative changes if present long term (11, 12)).
What’s the etiology?
LLD’s can be structural (anatomical) or functional (pathomechanics, compensation). LLD’s can be due to foot problems (overpronation/supination, fractures), leg or thigh problems (congenital shortening, deformity, fracture), or pelvic compensation (rotation of ilia, fractures).
So, what is the etiology? A lot can be gleaned from the history. Past trauma is the most obvious so pay close attention. This could result in flattening of the calcaneus or overpronation due to ligamentous laxity; tibial fractures can cause shortening as well as increased or decreased tibial torsion; similar findings can occur in the femur, along with anteversion or retroversion; pelvic trauma can be more subtle and x-ray can often provide the most information (1, 2, 4, 6).
How do you determine a leg length inequality?
There are a number of methods, each with their own merit. X –ray is most accurate, but exposes the patient to ionizing radiation. Weight bearing seems most appropriate, since symptomatology usually presents itself then. Supine measurements are said to be influenced by asymmetrical muscle tension, table pressure on the innominates and hip flexor length (15).
With the patient weight bearing and both feet placed below the trochanters, observe the level of the medial malleoli. Next, compare the heights of the tibial plateaus. Femoral length can be judged by the heights of the greater trochanters, and pelvic alignment judged by the heights of the iliac crests (4, 17).
Alternately, lay the person supine and observe the heels and medial malleoli. If there is noticeable discrepancy, they may have a short leg; if there isn’t, they still may have a discrepancy that they are compensating for. Check the range of motion of the foot and ankle in 6 general directions: plantar flexion (40-45 degrees), dorsiflexion (20-25 degrees, depending on whether the knee is flexed or extended), inversion of the forefoot (3-60 degrees, on average), and eversion of the forefoot (20-45 degrees on average), calcaneal inversion (4-20 degrees) and calcaneal eversion (4-10 degrees). Excessive calcaneal eversion usually means over pronation due to a longer leg on that side; excessive inversion can mean a long leg due to a cavus foot type (2, 4, 6, 8, 9, 12). Lack of flexibility in the posterior compartment of the calf usually causes a greater degree of pronation (16).
Now, perform Allis’s test. Bend both knees to 90 degrees and observe the height of the tibial plateaus. The lower one is usually the side of the discrepancy (which can be in tibial length or due to excessive pronation). Now walk superior to the knees and observe the femurs from more cephalad (4). Is there a discrepancy? If so, the problem may be in the femur length, femoral head angle or pelvis. Extend the knees so that the legs are lying flat on the exam table. Palpate the greater trochanters on both sides. Is one lower than the other? If so, they probably have coxa vara on the short side or coxa valga on the long side. If they are even, you need to look at the pelvis. Does one ASIS palpate more anterior or posterior than the other? This could represent compensation. A posterior or “flexed” ilia, usually causes a short leg on that side; an anterior or extended ilia usually causes a long leg on that side. Now stand the patient up and perform a Gillet Test. Have them stand erect and hold onto something for balance. Palpate the PSIS on one side along with the 2nd sacral tubercle. Have them raise their thigh to 90 degrees on the side you are palpating. The PSIS should nutate backward (flex) and drop .5-1.5 cm on the side of the raised leg. Now have them raise the opposite leg. The sacrum should nutate backward and down. If either of these movements does not occur, consider pelvic pathomechanics and treat accordingly. Recheck for motion as well as leg length when done.
Standing observation often (but not always) reveals overpronation on the long leg side and relative supination on the short leg side. The shoulder is often higher on the short side and the waistline dips to the long side because of posterior rotation of the innominate. The shoulder will dip to the side of the short leg on heel strike during dynamic evaluation (4, 6, 8, 9, 10, 11). Gait observation usually reveals adduction of the pelvis toward the stance phase leg with a lateral sway in excess of 1” during stance phase. The person will seem like they are “stepping into a hole” on the short side.
Conclusion
Leg length inequalities occur due to a variety of anatomical and physiological conditions. Careful analysis and examination can often reveal its etiology. To lift or not to lift is a clinical decision that is left to the clinician and patient, with a careful balance between what is perceived as improved biomechanics and tolerance levels of the patient with regards to their presenting symptomatology.
Resources
1 Cyriax J. Textbook of Orthopedic Medicine Vol I, 5th Ed. London: Baillare, Tyndall and Cassell, 1969
2 Taillard W. Lumbar Spine and Leg Length Inequality. Acta Orthop Belg 1969; 35: 601
3 Subotnick S. Case History of unilateral short leg with athletic overuse injury. JAPA 1980; 5: 255-256
4 Micahud T. Foot Orthoses and other forms of conservative foot care. Newton, MA 114-117: 1993
5 Martens M, Backaert M, et al. Chronic leg pain in athletes due to a recurrent compartment syndrome. Am J Sports Med 12: 148-151: 1984
6 Valmassey R. Clinical Biomechanics of the lower extremities. Mosby, St Louis, Philadelphia. 101-107: 1996
7 Press SJ. A report of clinical applications of computers in analysis of gait spinal imbalances. Chiro Sports Med 1987;1:30
8 Shawn Eno, personal communication
9 personal observation
10 Botte RR: An interpretation of the pronation syndrome and foot types of patients with low back pain. JAPA 71: 243-253, 1981
11 Friberg O: Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine 8: 643-651, 1983
12 Rothenberg RJ: Rheumatic disease aspects of leg length inequality. Sem Arth Rheum 17: 196-205, 1988
13 Travell J, Simons D. Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams and Wilkins 112, 1983
14 Schuit D, Adrian M, Pidcoe P. Effects of heel lifts on ground reactive force patterns in subjects with structural leg length discrepancies. Phys Ther 69(8): 41-48, 1989
15 Rothbart BA, Estabrook L. Excessive Pronation: a Major biomechanical determinant in the development of chondromalacia and pelvic lists. JMPT 5: 373-379, 1988
16 Kirby KA Effect of Heel Height Differential in Shoes on Orthosis Function. Precision Intracast Newsletter, March 1987, 1-3
17 Hoffmn KS, Hoffman LL. Effects of adding sacral base leveling to osteopathic manipulative treatment of back pain: A pilot study JAOA 94 (3): 217-220, 223-226 1994
18 Lee KH, Shieh JC, et al. Electromyographic changes of leg muscles with heel lifts in women: therapeutic implications. Arch Phys Med Rehabil 71(1): 31-3, 1990
19 Lee KH, Matteliano A, et al. Electromyographic changes of leg muscles with heel lift: therapeutic implications Arch Phys Med Rehabil 68(5 pt 1): 298-301, 1987
20 McCrory JL, White SC, Lifeso RM: Vertical ground reaction forces: objective measures of gait following hip arthroplasty Gait Posture 14(2): 104-109, 2001
21 Blake RL, Fregeson HJ. Correlation between limb length discrepancy and assymetrical rearfoot position JAPA 83(11): 625-33, 1993
22 Song KM, Halliday SE, Little DG. The effect of limb length discrepancy on gait. J Bone Joint Surg 79(11): 1160-1168, 1997
The Toe Waving Exercise, Part 2
In part one of this series, we talked about the importance of the short flexors of the toes (FDB or flexor digitorum brevis) in forming and maintaining the foot tripod. In this installment, we discuss another important muscle used in this exercise, the extensor digitorum longus (EDL).
We have shown you time and time again, dominance of the long flexors in gait, which cause biomechanical imbalances. We remember that through reciprocal inhibition, the log flexors will reciprocally inhibit the long extensors, so increased activity in the former, means decreased activity and activation in the latter.
The balanced activity of the long flexors and long extensors helps to create harmony during gait. Working the long extensors with this exercise (along with others, like tripod standing, toes up walking and the shuffle gait exercises) helps one to achieve this balance.
The Gait Guys; promoting foot and gait competency every day here, on Youtube, Facebook, Twitter, and in our offices and yours.
all material copyright 2012 The Homunculus Group/The Gait Guys. All rights reserved. If you rip off our stuff, you will never have an adequate foot tripod and will have gait problems for the remainder of your days.
Somnambulation (Sleepwalking). Gait and sleepwalkers.
/Sleepwalking. Are you asleep or are you awake ? Which is it ? Or is it both?
Aspects of non-rapid eye movement (NREM) sleep and wakefulness can occur simultaneously in different parts of the cortex in mammals, including humans.
According to wikipedia:
Sleepwalking, also known as somnambulism, is a sleep disorder belonging to the parasomnia family.Sleepwalkers arise from the slow wave sleep stage in a state of low consciousness and perform activities that are usually performed during a state of full consciousness. These activities can be as benign as sitting up in bed, walking to the bathroom, and cleaning, or as hazardous as cooking, driving, having sex, violent gestures, grabbing at hallucinated objects, or even homicide.
“sleep is considered a global brain and behavioral state. However, recent intracortical recordings have shown that aspects of non-rapid eye movement (NREM) sleep and wakefulness can occur simultaneously in different parts of the cortex in mammals, including humans. Paradoxically, however, NREM sleep still manifests as a global behavioral shutdown.”
Abstract: A case of childhood-onset somnambulism is reported in which a 43-year-old man presented with repeated sleep-related injuries incurred during violent nocturnal activity, which included frenzied running, throwing punches and wielding knives. He had also driven an automobile a long distance during a presumed somnambulistic state. His wife had been repeatedly injured, and she felt that her life was threatened by his nocturnal violence 2-3 times yearly. Polysomnography (PSG) documented multiple episodes of complex and violent behaviors arising exclusively from stage ¾ sleep, thus confirming the diagnosis of somnambulism.
Season 1: Podcast 8 of the Gait Guys Experience Now available!
/You know you want it! Here it is:
You can check it out on Libsyn, by clicking here:
This link will get you a nicely laid out “show notes” and pod player.
http://thegaitguys.libsyn.com/the-gait-guys-experience-podcast-8-s1e8
This one will get you to the show player of ALL of our podcasts.
http://directory.libsyn.com/shows/view/id/thegaitguys
Here are the show liner notes:
1- neuroscience story
What do dolphins and sleep walking have in common?
Do ultra marathoners sleep while they run ?
Join us for the podcast neuroscience introduction.
2- More lectures available on www.onlineCE.com 13 hours of courses there ! Go there and look up our lectures
3- OFF TOPIC Discussion:
So many of them supinate and have a wide tripod…….
Julio C, in Sao Palo Brazil !
5- EMAIL Question:
Hi!
6- EMAIL CASE:
Guys, love you, love your show
Anyhow…….enough ego stroking…….
What is your take on the biomechanical implications of a short quadriceps muscle in gait ?
7- Pedographs or software ???? what is our take ?
8- EMAIL CASE
Hi Fellas
You talked about it several blog posts but i would love to hear you expand upon it.
thanks
Jordan
9- EMAIL:
Is it true that walking in flip flops is bad for you? I’ve heard a lot of “experts” say it will cause your arches to fall. Thanks! - Norma
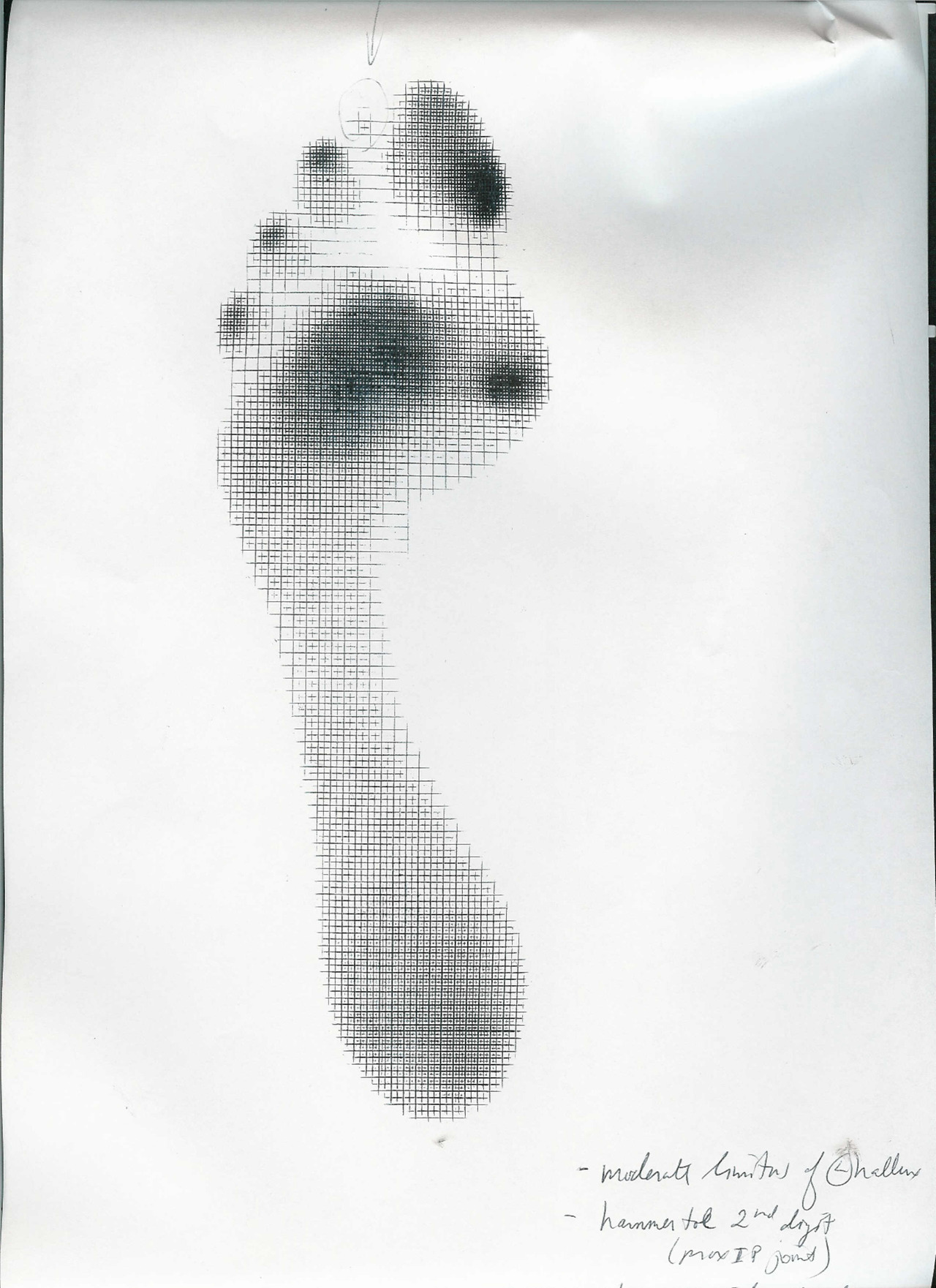
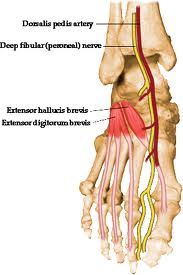
The Mighty Extensor Digitorum Longus (EDL): a pedograph case.
We have long been promoting appropriate function of the long extensors of the toes (predominantly the EDL, but also the Extensor hallucis longus) here, in our practices, our lectures, on Youtube, in our book……You get the idea. Lets tale a closer look at this muscle (picture left above)
The EDL has a proximal attachment in the lower leg up at the condyle of the tibia, proximal fibula, the interosseus membrane, and the connective tissues between the muscles. It travels down the leg, under the extensor retinaculum and attach to the base of the distal phalanges of toes 2-4. These muscles act from initial contact (to help eccentrically lower the foot to the ground), loading response (to continue to lower the foot slow or attenuate pronation), midstance and terminal stance (to provide compression of the metatarsal phalangeal and interphalangeal joints, and to offset the long flexors (which are often overactive, due to flexor dominance)).
What does it look like when the long extensors don’t work so well? Have a look at the pedograph on the right. what do we see? First we notice the lack of printing under the head of the 1st metatarsal and increased printing of the second metatrsal head. Looks like this individual has an uncompensated forefoot varus (cannot get the head of the 1st metatarsal to the ground, and thus a weak medial tripod). Next we see increased printing of the distal phalanges of digits 2-4. Looks like the long flexors are dominant, which means the long extensors are inhibited. What about the lack of printing of the 5th toe? I thought the flexors were overactive? They are, but due to the forfoot varus, the foot is tipped to the inside and the 5th barely contacts the ground!
How do you fix this?
Help make a better foot tripod using the toe wave, tripod standing and extensor hallucis brevis exercises. Make sure the articulations are mobile with joint mobilization, manipulation and massage. Make sure the knee and hip are functioning appropriately. Give the client lots of homework and put them in footwear that will allow the foot to function better (a less rigid, less ramp delta shoe). As a last resort, if they cannot make an adequate tripod (because of lack of motivation or anatomical constraints), use a foot leveling orthotic.
Ivo and Shawn. Two guys, making a difference, every day.
all material copyright 2012 The Homunculus Group/The Gait Guys. All rights reserved. If you rip off our stuff, you will be plagued with foot fungus and bunions for all your days.
Torsions
This gentleman has 2 excellent examples of thing you will see commonly: femoral retrotorsion and internal tibial torsion.
The neck of the femur usually makes an 8-25 degree angle (average 18 degrees) with the shaft of the femur. If this is greater than 25 degrees it results in a condition called femoral antetorsion and if less than 8 degrees, it is called femoral retrotorsion.
Femoral retrotorsion results in one having LESS internal rotation of the hip (and increased external rotation) and femoral antetorsion results in having a GREATER amount of internal rotation (and less external rotation).
We normally need 4 degrees of internal rotation of the hip to walk normally. Most people have at least 40 degrees. Look at the shots above of this gentleman who has almost zero. This range of motion needs to come from somewhere, and in this individual, it is occurring at the foot (in the form of a “spin” with gait, and complimentary tight achilles tendons).
Now look at the alignment of the tibial tuberosity with the lower leg. See how it faces medially? It should be about 22 degrees in the adult. More than this is called external tibial torsion and less (like here) is internal tibial torsion. Note how the foot is “toed in” on both sides? This will keep the foot in supination longer and you will weight the outside of the foot more. Put a conventional orthotic on this person without forefoot valgus posting and you are asking for a meniscus problem!
Now look at the “bow” (or varum, as it is called) of the tibia. Normal here is 4-6 degrees and he is in excess of 10. You will often see this in clients with internal tibial torsion.
So, what’s the fix?
You could do a surgery, like they did to Ethan Hawke in “Gattica” or you could make sure the foot has an adequate tripod (which this client did not). Tripod exercises (coming soon on the blog), EHB exercises, Toe waving exercises are all important, as well as foot, knee and hip manipulation to assure normal mechanics are present. Make sure that hip internal rotation is adequate and that gluteus medius and minimus finction is appropriate, as well as vastus lateralis (yes, lateralis is an INTERNAL ROTATOR when the foot is on the ground).
Torsions. Hope you are seeing these as much as we are.
Your twisted Gait Geeks; Ivo and Shawn
The Toe Waving Exercise: Part 1
Welcome to Friday, Folks. A little exercise here for you today that we use all the time.
There are at least 3 muscles important in forming and maintaining the foot tripod. The short flexors of the lesser digits (Flexor Digitorum Brevis or FDB) are one of the important component sfor creating and maintaining the foot tripod (the tripod between the head of the 1st metatarsal, head of 5th metatarsal and center of calcaneus).
It arises by a narrow tendon from the medial process of the calcaneal tuberosity the plantar aponeurosis, and from the connective tissue between it and the adjacent muscles. As it passes forward, and divides into four tendons, one for each of the four lesser toes which divide into 2 slips ( to allow the long flexor tendons to pass through), unite and divides a second time, inserting into the sides of the second phalanx.
Because the axes of the tendons passe anterior to the metatarsal phaalngeal joint (MTP), they also provide an upward (or dorsal) movement of the MTP joint complex, moving it posterior (or dorsal) with respect to the 1st metatarsal heal (thus functionally moving the 1st met head “down”). This is a boon for people with a forefoot varus, as it can help create more mobility of the 1st ray, as well as help descend the head of 1st ray to form the medial tripod (and assist the peroneus longus in anchoring the base of the big toe). It also helps the lumbricals to promote flexion of the toes at the MTP, rather than the distal interphalangeal joint.
In this brief video, Dr Ivo explains the exercise to a patient (Thank you N, for allowing us to use this footage).
The Toe Wave: try it. Use it with your patients. Spread the tripod. We know you want to….
Ivo and Shawn
all material copyright 2012: The Homunculus Group/The Gait Guys
Using a Pedograph to get Dynamic Answers to Foot Dysfunction:
Pedograph topic: One quick topic here. Note the hot spot (ink concentration) at the big toe and note that the ink is proximal on the toe pad. We would like to see the pressure point at the center of the pad. This spot means this person walked across the Harris Ink mat with increased FHB (flexor hallucis brevis) use and not enough FHL (flexor hallucis longus); too much short flexor, not enough long flexor. There is loss of synergy between the two. This will likely mean there is something going on in the extensors as well, something abnormal.
Need a review? Look at Monday’s video again on the EHB (extensor hallucis brevis) where we discuss all of the toes muscles.
Clinically this patient had a hallux limitus/rigidus (could not dorsiflex great toe) which complicated the mechanics at the joint and forward into the great toe, sadly also at the foot’s medial tripod as well. You cannot get an accurate read from a static (standing only) pressure mapping. Don’t rely on them for dynamic info !
Too much FHB with not enough FHL means EHB (as well as long extensors of the lesser toes) is going to be impaired. Impair the EHB and you ask the EHL to work differently as well. Here’s a hint, look at all the printing under the lesser digits distally, there is too much flexor activity here as indicated by intense inking from toe clenching / hammering. They are likely doing this to add more stability since the great toe cannot from what we discussed above. There are problems that come from these issues as well but we want to stay focused on the big toe today.
Now, go back and review Mondays blog video post (here is the link).
Treatment:
In a case where there is some loss of the 1st MPJ range of motion (metatarsaphalangeal joint) (depending on the source, 45 degrees is typically needed) there will be impairment of the long and short toe flexor/extensor pairing and synergy. In this case above there is highly suspected increased short flexor (FHB) activity (hence the ink at the proximal big toe) and this means that the long flexor is usually submissive. And, when the long flexor (FHL) is submissive the long extensor is dominant. When the long extensor is dominant the short extensor is submissive. Can you now see the beautiful symphony and harmony we need here. This is why we loosely say that the FHB and the EHL are paired and the FHL and EHB are paired. It is not exactly the case but hopefully you catch our drift.
So, in this case, with a hallux limitus/rigidus when the 45 degrees of dorsiflexion is lost these pairing can be challenges and the synergy is lost. The symphony of these muscles is “off tune”. This can further provoke the 1st MPJ and it can also be the slow brewing initiation of the problem. It can be a vicious cycle when it gets going. And, when the 1st MPJ is limited the dorsiflexion that is supposed to occur at the joint can be shunted proximally into the midfoot or ankle and cause pain/pathology there. It can also impair the normal pronation-supination cycles. The big toe when it goes sour makes the whole orchestra angry and play off tune.
Doing your best to normalize and maximize muscle harmony and function many times will dampen the pathology and pain and get the person going again. Of course the problem is still lurking under the surface. Test the muscles, try to isolate them but remember that your muscle tests need to be as specific as you can. Nothing is isolated in the body, but do your best.
Of course there are many other scenarios but this is the one we chose to teach today from this pedographing of the big toe. We will explore other options and challenges another time.
Shawn and Ivo. Gait geeks promoting gait literacy and competency everywhere we can get an open ear.
EHB: Extensor Hallucis Brevis
/
The Gait Guys Podcast #7: S1E7
/This one will get you to the show player of all of our podcasts.
http://directory.libsyn.com/shows/view/id/thegaitguys
And this link will get you a nicely laid out “show notes”.
http://thegaitguys.libsyn.com/webpage/2012/08
Show Notes: The Gait Guys Podcast, Season 1, Episode 6
1- CPR: neurscience story
http://www.bbc.co.uk/news/health-15552957
Correctly performed CPR triples survival rates. The UK Resuscitation Council recommends that the chest should be compressed by 5-6 cm and at a rate of 100-120 compressions per minute. A study published in 2009 showed that using a familiar song as an AID did increase the number of people getting the right rate. But there was a drop in those hitting the correct depth.
3. - EMAIL CASE:
off our FB page, from Lisa
I’m so hoping you can help me out with a patient. He is a military runner (Army) who hope to compete his first full Tri this year. In a nutshell: He has been plagued with peroneus Longus pain on his slightly longer side with running. This now occurs only with running in the combat boots and he uses a Nike Free Boot. I have checked all shoes for manufacturer defects.
Barefoot running, ankle rocker exercises, Glu. med strengthening for cross-over gait have helped his out of boot running experience, but he is frustrated by calf pain in the boots and so am I. I do have a video gait barefoot that I can send you. We have discussed the problem of trying to be a midfoot striker in a boot.
He does the waddle gait w/ theraband, squats with toes up, shuffle gait and moonwalk backwards. As far as i know, the military has banned VFFs for training and maybe all minimalist shoes. Scratching head…
What is thought to happen is that one partner dominates the lead in the gait, just as in dancing, one person is the leader and the other is the follower. The lead partner’s lower limbs determine the movement of their arms, which in turn when holding hands, sets the arm movement pattern in the partner then determining the leg swing and stance phases. Thus, synchrony is achieved.
References used:
J Neuroengineering Rehabil. 2007; 4: 28. The sensory feedback mechanisms enabling couples to walk synchronously. An initial investigation. Ari Z Zivotofsky and Jeffrey M Hausdorff Published online 2007 August 8. doi: 10.1186/1743-0003-4-28
- So a bit of background, i am a 28 year old very keen amateur (2.23 marathon) who has a 5 year history of heavy run training (80-120 miles per week) having been a triathlete prior to that and a swimmer from the age of 8. I had no injury history prior to this except, perhaps crucially, in 2006 i twisted my right ankle into supination, several times over the course of 2-4 months, I never had to stop running for more than a day or two at this time but it was very swollen and for at least 6 months was very unstable, but i ran through it.
- so current injury is a 2.5 years of vague right posterolateral gluteal pain which is constantly there but progresses with running to a spasm, over the area i believe to be the glute medius and some mild adductor pain on the same right hand . . i can usually get through easy mileage but the pain is always there and speed work/racing is a no no. I had bilateral sports hernia surgery on the 3rd january in the belief that it would cure the problem , it helped and certainly reduced the abdominal/adductor aspect but i still cant race and I know think the sports hernias were a product of the problem and not the problems route cause.
- I have no problems on the left. my right foot are some callouses on the right on the medial aspect of the arch.just proximal to the 1st MTP
- the navicular is much more prominent on the right.
the foot wear pattern on the right shoe is different, there appears to be a far heavier heel strike on the right lateral side, greater wear under where the right 1st MTP joint would be.
-
on the left there is far more “toe off” wear on the shoe after periods of inactivity it feels as though the foot needs to warm up before it will pronate sufficiently to allow toe off. like im walking on the outside of the foot.
-
the right hip has more internal rotation and less external rotation than the left,
-
flexion and extension at the hip are stiff but within i believe normal limits.
-
the hallux tests i have found online dont appear to show any restricton although i was initially cheating on the right with foot pronation.
- the podiatrist said I had bilateral forefoot varus with it being worse on the right. he noted my prominent naviculars, he initially thought I had accesory bones but confirmed that i did not. he said that on the right (my bad leg) had a restriction/fixed at the midtarsal joint so the increased required pronation to get the first ray down had to come from sub-talar pronation.
- onto the walking pressure pad analysis,
-on the right (bad leg) i had alot of lateral edge mid foot loading, the right foot was much more externally rotated than the left.-on my left leg the peak force/pressure was very unusally right under the tip if the hallux-on the right the forces were much less throught the heel strike, stance, and push off phaseonto the video analysis.
when you slow down my gait the left (my good, pain free leg) looks incredibly odd.on the “swing through” phase (so when my right was on the floor) my left knee points laterally and appears to circumduct through rather than progress straight in the saggital (?) plane. as the left foot approached foot strike is looks much more supinated than the right.-this is in contrast to my right (painful leg) which swung though perfectly in the saggital plane,-no movement laterally in the frontal plane, no cicumduction, approached foot strike with much less supination and just looked mor normal.
The podiatrist thinks all my problems are coming from my left foot, despite that being my good leg. so he gave me a knocked up orthotic to use in my left shoe which basically pushes me more into supination at the arch and calcaneus, nothing in the forefoot. he thought there was nothing to do in the right foot.he told me to try it for 6 weeks and if it worked he would prepare a more robust permanent version.This is where my questions came from the things I have learnt from the gaitguys, Basically i questioned why if I have a forefoot varus is there nothing in the forefoot to bring the ground up to the first ray. and help attenuate the subtalar pronation on the right and mid tarsal/subtalar joint on the left. he said through years of experience, which is fair enough of an answer as I dont have any experience or qualifications of my own!I enjoyed the assessment and I thought it was enlightening but cant help but feel he mar be very good at detecting/ diagnosing but im not convinced that his remedy is the way forward.Despite the abberent movements of the left leg Im still convinced the right is the problem and what i see in the left in swing though is a product of poor mechanics of the right foot when its on the floor.Thanks again. Nathaniel , United Kingdom
The Gait Guys www.onlineCE.com courses.
/https://chirocredit.com/courses/index.php?catid=124&pid=1
Biomechanics
Biomechanics 208 Case Studies in Gait Analysis: Challenges to the Knee during Gait
Credit Hour(s): 1.0
Educational Objectives:
Review the pertinent anatomy of the knee
- Review the kinematics and kinetics of knee function during the gait cycle
- View and discuss case studies involving knee function
- Predict pathomechanics that will arise from the gait abnormalities presented
- Propose remedies for the gait abnormalities seen
Format(s):Adobe PDF Download Android Compatible
Slides with audio
Price:$20.00 USD
Biomechanics 207 A case study in gait analysis: focus on torsions and versions
Credit Hour(s):1.0
Educational Objectives:
- Assess actions of the lower kinetic chain during gait
- Predict pathomechanics that will arise from gait abnormalities presented
- Propose remedies for the gait abnormalities seen
- Review the gait cycle and gait cycle biomechanics
- View and discuss case studies of gait
Format(s):
Android Compatible
Ipad/Iphone compatible using Puffin Browser
Slides with audio
Price:$20.00 USD
Biomechanics 206 A Case Study in Gait Analysis
Credit Hour(s): 1.0
Educational Objectives:
- Review the gait cycle and gait cycle biomechanics
- View and discuss case studies of gait
- Assess actions of the lower kinetic chain during gait
- Predict pathomechanics that will arise from gait abnormalities presented
- Propose remedies for the gait abnormalities seen
Format(s):
Android Compatible
Ipad/Iphone compatible using Puffin Browser
Slides with audio
Price:$20.00 USD
Biomechanics 205: Barefoot Running and Gait: What you need to know
Credit Hour(s):1.0
Educational Objectives:
- Explore barefoot running from a position of biomechanical efficiency
- Contrast the differences in shod vs unshod running
- Predict problems that can arise from shod and barefoot running
- Apply visual analysis skills to barefoot running technique
- Describe how to introduce barefoot running to your patient population
Format(s):
Android Compatible
Ipad/Iphone compatible using Puffin Browser
Slides with audio
Price:$20.00 USD
Biomechanics 204: Shoe selection and the effect and impact on gait
Credit Hour(s):1.0
Educational Objectives:
- Describe and identify how the parts of a running shoe affect running biomechanics
- Compare and contrast different shoe constructions to the biomechanical needs of an individual
- Determine the appropriate last shape for different foot types
- Discuss the biomechanical consequences of improper vs. proper selection of last types
- Predict which features in a shoe are necessary to correct faulty gait patterns
Format(s):
Android Compatible
Ipad/Iphone compatible using Puffin Browser
Video Presentation
Price:$20.00 USD
Biomechanics 203:Gait Analysis: Normal and Abnormal Gait and factors affecting them
Credit Hour(s):3.0
Educational Objectives:
- Discuss the normal walking gait cycle
- Apply the biomechanics of the pelvis and lower kinetic chain during walking to clinical practice
- Predict and discuss problems and clinical strategies that can arise from altered lower extremity biomechanics
- Apply visual analysis skills
- Evaluate case studies in gait analysis
- Clinically apply solutions for gait abnormalities
Format(s):Adobe PDF Download
Ipad/Iphone compatible using Puffin Browser
Video Presentation
Price:$60.00 USD
Biomechanics 202:Foot Function and the Effects on the Core and Body Dynamics
Credit Hour(s):1.0
Educational Objectives:
- Describe how the motor and sensory homunculus relate to the foot and are integral to training and rehabilitation
- Discuss the 3 rockers of the foot
- Give examples of problems that result from a loss of the 3 rockers of the foot
- Explain the concept of pelvis neutrality and its effect on training
- Describe and examine the tripod of the foot
- Breakdown most movement into 2 basic rules or tenets
- Give examples of the problems which can arise if the 2 basic rules or tenets of movement are not followed
- Discuss the clinical consequences of loss of the medial and lateral tripods of the foot
Format(s):
Ipad/Iphone compatible using Puffin Browser
Video Presentation
Price:$20.00 USD
Biomechanics 201: Introduction to Gait: Pedographs and Gait Analysis
Credit Hour(s):4.0
Educational Objectives:
- Explain the phases of human walking gait
- Discuss the biomechanical events associated with stance phase of gait
- Discuss the biomechanical events associated with swing phase of gait
- Explain biomechanically what is happening during each phase of gait in the foot, ankle, knee and hip
- Discuss the 3 rockers of the foot and how they apply to the gait cycle
- Understand the calcaneocuboid locking mechanism and defend it’s importance in the stance phase of gait
- Summarize the ranges of motion of the foot, ankle, knee and hip and their importance in normal gait
- Explain how stance phase abnormalities would impact the gait cycle
- Demonstrate competency in obtaining a reproducible Pedograph print
- Interpret rearfoot, midfoot and forefoot mechanics as seen on a pedograph print
- Identify and interpret problem areas in a pedograph print
- Identify stance phase abnormalities on a Pedograph print
- Extrapolate pathomechanics which would occur rostrally in the kinetic chain during pathomechanics occurring in the gait cycle
- Evaluate the impact of gait abnormalities on human locomotion
Format(s):
Iphone/Ipad Compatible
Price:$80.00 USD
Runners . . . On Your Mark, Ready, Set.....Swim.
/For many of the years of my youth I watched just about every NBA basketball game I could get my eyes on. When I wasn’t dreaming of playing ball in the big time I was at the local YMCA in my small town shooting jump shots, working on my fading jumper (because i was a small guard with no vertical, the worst of combinations), and working on my ball handling techniques. I was not a great player, not by any means, but I could play in pretty competitive pick up games and at least be somewhat respectable (note that ‘somewhat’ is highlighted). But I still dreamed big about the NBA until I became old enough to realize that I was just too short and not blessed with the natural talent for the game that others obviously had been blessed. No matter how much I dreamed, being 5 foot 8 inches wasn’t going to ever get me to the big dance. Body type, form, physiology and your anatomy have a big part in what sport you will be good at. There just are not too many 5'8" NBA guards, there never were minus Mugsy and Spud. They were an exception, obvious outliers.
Are you a runner with runner’s anatomy ? Do you have bowed legs ? Forefoot varus flat feet ? Anteverted hips ? Excessive tibial torsion ? These are not great traits for runners. They tend to lead to many biomechanical issues that provoke injury at a much higher incidence than someone like my friend Charlie Kern , the USA masters mile champion. Charlie is like Tiger Woods. Charlie has straight lower limb bones, no bony versions or torsions, great feet, he is slender, excellent muscle structure, and has tons of natural ability. If you have ever seen him run it is like watching water flow. Charlie is as a runner just like Tiger is as a golfing Ferrari. They both happened to pick a sport that their body’s were perfectly suited for, then they had the passion for that sport, were lucky to have found it at a young age, and they worked harder than anyone else at their sport. Anatomy, a bit of luck in sport choice early on, a physiology that paired well with the anatomy, and a work ethic to trump anyone. Being the best is a combination of things. You can have all the desire in the world as a runner or athlete but if you do not have the magic mixture of all things necessary you might just be average instead of extraordinary.
Do you get injured all the time when you run ? How are your feet, are they competent or are they flat ? Do your tibias bow like a weathered piece of lumber ? Are your knees kinked inwards (genu valgum) ? Are you tall and thin or are you build like a line backer ? In other words, are you suited to be a distance runner or marathoner ? Or should you be happy with three to four 5k runs a week and be happy you can run those smaller distances rather than spend every 2 weeks in the therapists office getting a foot fixed, an orthotic tweaked, kinesiotape on a knee, more rehab. Do you spend more time icing your injuries and doing pre-run theapeutic exercises and foam rolling than you do running ?
If this is you. God bless your dedicated heart. But maybe you should put on your Speedo and go for a swim. I put my NBA dreams on hold long ago after realizing that at 5'8" it just wasnt going to happen. I picked up golf and did much better at that game in a shorter period of time than all the work on my hoop dreams. I would fathom to say I should have picked up ping-pong long ago as a child. Perhaps I would be world champ by this time.
Run, bike, swim, hoops, golf…..whatever your passion. There is nothing wrong with having heart and grinding it out daily to be a runner or do whatever your sport happens to be. Just never lose sight of the obvious. Maybe you need to look past your heart and look in the mirror and your mounting therapy bills and make some adjustments to your running dreams. Some of my best Triathletes were awesome runners at one time … . when we could get them healthy to a start line line. The problem was that they had more unused race bibs than completed races. They were in my office regularly pleading me to fix them up so they could get their training in so they could get to race day. However, after much psychoanalysis and reality talking we finally got through to some of the best athletes. Once we switched them to triathlons where they could moderate the runs and hit some alternative sports that did not play up their challenged race anatomy, they rose to the top and rarely had to hand off a race bib to a friend who was healthy. And they are happier. I see them far less in my office and far more at the finish lines with a huge smile.
Do some honest inventory of your body. Sometimes a Speedo just makes sense, well, sort of. If you catch our drift.
Dr. Shawn Allen, The Gait Guys
Did you know that the EHB (extensor hallucis brevis) the topic of today’s video tutorial, originates off of the forepart of the medial aspect of calcaneus & lateral talocalcaneal ligament. It is just above the bulk origin of the EDB (extens
Part 2 of the EHB: Bringing the Extensor Hallucis Brevis of the Foot Back to Life.
Today we show you a proprietary exercise we developed here at The Gait Guys. It was developed out of necessity for those clients who are too EHL dominant (long big toe extensor muscle) and big toe short flexor dominant (FHB). These two muscles are what we call a foot functional pair. Big toes like these will be dysfunctional and will not be able to gain sufficient purchase on the ground to produce stability and power without impacting the joint (1st metatarsophalangeal joint). Imbalances like these lead to altered joint loading responses and can be a possible predictor for premature damage to the joint over time. These imbalances are also what lead to injuries to the big toe, the arch and other areas of the foot. After all, when the big is weak or dysfunctional gait will be compensated. When imbalance at this joint occurs because of EHB weakness the medial tripod anchor (the head of the 1st metatarsal) is compromised possibly transmitting stress into the foot, arch and medial stabilizers such as the tibialis posterior for example.
This exercise is to be weaned back to less and less yellow band resistance until the EHB can be engaged on its own. Then the gait retraining must begin. Simply reactivating and strengthening the skill and muscle is not enough. The pattern must be then taken to the floor and learned how to be used in the gait cycle.
Do we need to mention the critical function this muscle plays in extension of the 1st MPJ, of its importance in hallux rigidus/limitus, in bunions, hallux valgus, toe off function, arch height and function ? We hope not.
It is a process restoring gait. All too often the “Devil is in the Details”.
If you liked this video, visit our daily blog: www.thegaitguys.tumblr.com
or our website: www.thegaitguys.com
See our other free videos here on youtube on our “The Gait Guys Channel”.
Or our other videos here: http://store.payloadz.com/results/results.asp?m=80204
Shawn and Ivo
The Gait Guys
all material copyright 2012 The Gait Guys/ The Homunculus Group: all rights reserved.
Classic Crossover Gait Case.
Here is a client with a uncompensated forefoot varus (ie: the forefoot is inverted with respect to the rearfoot) and a cross over gait, secondary to incompetence of the medial tripod of the foot (he cannot descend the head of his 1st metatarsal to form the medial tripod due to the uncompensated forefoot varus) and weak right lower abdominal external obliques which we discovered on examination (perhaps you can detect a subtle sag of the right side during stance phase on that side).
Note how he circumducts the lower extremities around each other. This takes the cross over to another level and it can occur when a client is pronating through the medial tripod such as in this forefoot varus case (we know this from the examination, it cannot be detected for sure from the video with the foot in the shoe, that would be an assumption).
How do you fix this?
- tripod standing exercises
- core stabilization exercises with attention to the right lower oblique (see our core series available for download on Payloadz here and here
- foot manual therapy to improve motion of the 1st ray
- see our crossover gait series on youtube here: part 1, part 2, and part 3
- form running classes such as Chi Running
The Gait Guys. Bringing you the meat, without the fat.
all material copyright 2012 The Gait Guys/ The Homunculus Group: all rights reserved
READY
The Gait Guys Case of the week: What do you see?
This individual presents with Right achilles tendonitis, bilateral foot pain and a history of plantar fascitis. What do you think?
Take a look at his foot type, particularly the forefoot to rearfoot orientation. Hmmm….Asymmetrical. Notice the dropped 1st metatarsal on the left that is not present on the right. He has a forefoot valgus on the left with a quasi flexible 1st ray (1st ray = medial cuneiform, 1st metatarsal and associated phalanges) which is dropped and an uncompensated forefoot valgus on the right, with an inflexible 1st ray.
He has bilateral external tibial torsion (which you cannot see in these pictures) right greater than left (OK, you can see that), as well as a Left anatomically short leg (tibial) of approximately 7mm.
Now look at the pedographs. BIG difference from left to right. Good tripod on right with clear markings over the calcaneus, the head of 5th metetarsal and the head of 1st metatarsals. But I thought you said he had an UNCOMPENSATED forefoot valgus ? Look at the shape of the forefoot print. It is very different from right to left. Remember, with a forefoot valgus, the medial side of the foot hits the ground before the lateral side most of the time,
How about the left? Look at all that metatarsal pressure. Looks like a loss of ankle rocker. Think that might be causing some of that left sided foot pain? Notice the print under the 1st metatarsal is even greater; and look at all that printing of the 5th metatarsal head. Remember, this is the shorter leg side, so this foot will have a tendency to supinate more, thus he increased pressures laterally.
Achilles tendonitis? Stand on one leg on your foot tripod and rock between the head of your 1st metatrsal and head of the 5th. Where do you feel the strain? The gastroc/soleus and peroneals. Now put all your weight on the lead of the 1st metatarsal. What do you notice? The foot is everted. What everts the foot? The peroneals. So, if the foot is everted (like in the forefoot valgus), what muscle is left to shoulder the load? Remember also, that the gatroc/soleus group contracts from mid to late stance phase to invert the heel and assist with supination of the foot.
The Gait Guys. Your guiding light to gait literacy and competency.
Want to know more about pedographs? Get a copy of our book here.
All material copyright 2012 The Gait Guys/The Homunculus Group.