Falling hard; Using supination to stop the drop.
“One thing, affects all things. One change necessitates global change. The more you know, the more you will see (and understand). The more you know, see and understand, the more responsible you will and should feel to get it right and the more global your approach should become. If your head does not spin at times with all the issues that need to be juggled, you are likely not seeing all the issues you should be seeing.” -Dr. Allen (from an upcoming CME course)
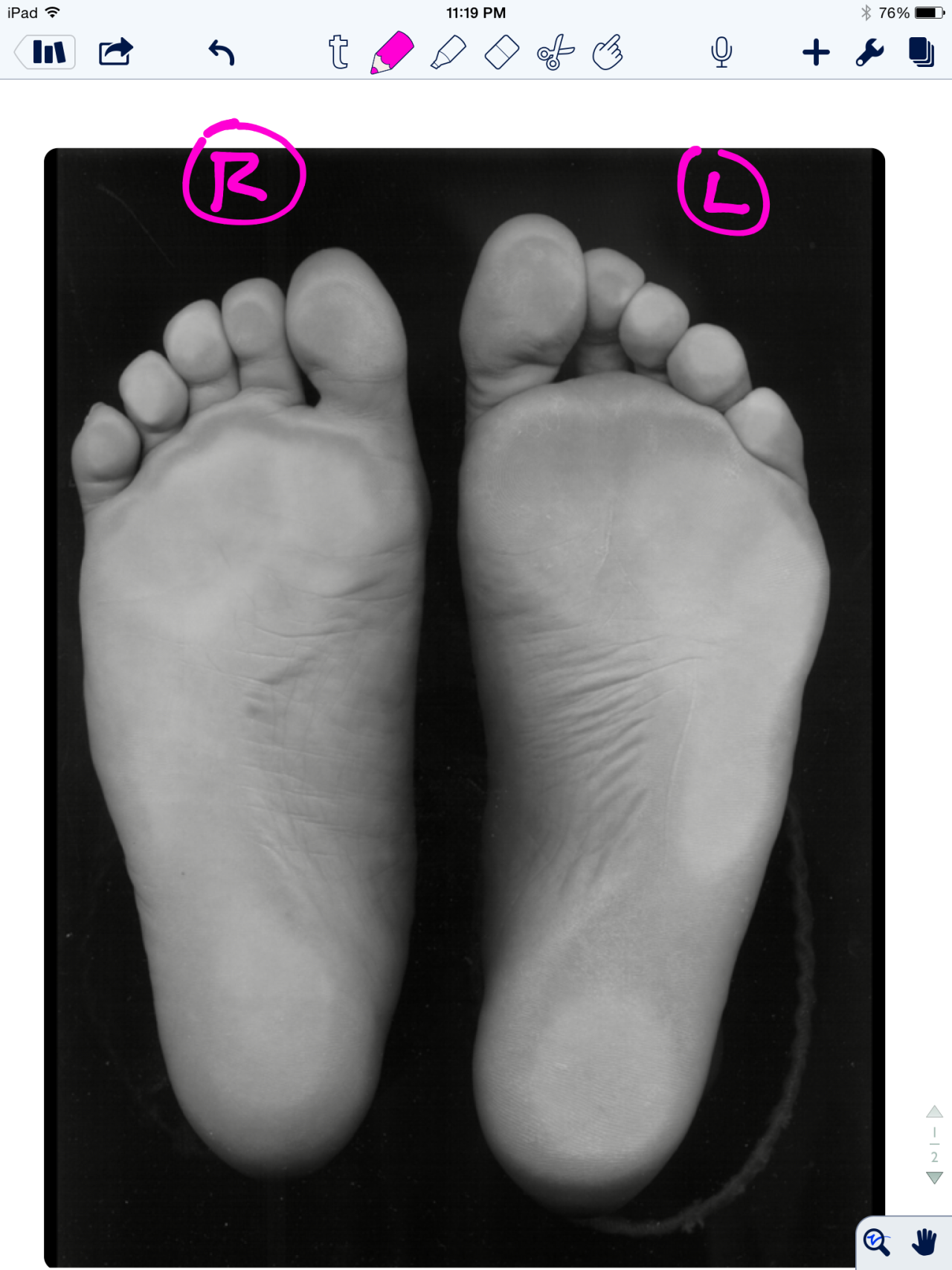
This is a case that has been looked at before but today with new video. This is a client with a known anatomic short leg on the right (sock-less foot) from a diseased right hip joint.
In this video, it is clear to see the subconscious brain attempting to lengthen the right leg by right foot strike laterally (in supination) in an attempt to keep the arch and talus as high as possible. Supination should raise the arch and thus the resting height of the talus, which will functionally lengthen the leg. This is great for the early stance phase of gait and help to normalize pelvis symmetry, however, it will certainly result in (as seen in this video) a sudden late stance phase pronation event as they move over to the medial foot for toe off. Pronation will occur abruptly and excessively, which can have its own set of biomechanical compensations all the way up the chain, from metatarsal stress responses and plantar fasciitis to hip rotational pathologies. It will also result in a sudden plummet downwards back into the anatomic short leg as the functional lengthening strategy is aborted out of necessity to move forward.
This is a case where use of a full length sole lift is imperative at all times. The closer you get to normalizing the functional length, the less you need to worry about controlling pronation with a controlling orthotic (controlling rate and extent of arch drop in many cases). Do not use a heel lift only in these cases, you can see this client is already rushing quickly into forefoot loading from the issues at hand, the last thing you should be doing is plantarflexing the foot-ankle and helping them get to the forefoot even faster ! This will cause toe hammering and gripping and set the client up for further risk to fat pat displacement, abnormal metatarsal loading, challenges to the lumbricals as well as imbalances in the harmony of the long and short flexors and extensors (ie. hammer toes).
How much do you lift ? Be patient, go little by little. Give time for adaptation. Gauge the amount on improved function, not trying to match the right and the left precisely, after all the two hips are not the same to begin with. So go with cleaner function over choosing matching equal leg lengths. Give time for compensatory adaptation, it is going to take time.
Finally, do not forget that these types of clients will always need therapy and retraining of normal ankle rocker and hip extension mechanics as well as lumbopelvic stability (because they will be most likely be dumping into anterior pelvic tilt and knee flexion during the sudden forefoot loading in the late midstance phase of gait). So ramp up those lower abdominals (especially on the right) !
Oh, and do not forget that left arm swing will be all distorted since it pairs with this right limp challenge. Leave those therapeutic issues to the end, they will not change until they see more equal functional leg lengths. This is why we say never (ok, almost never) retrain arm swing until you know you have two closely symmetrical lower limbs. Otherwise you will be teaching them to compensate on an already faulty motor compensation. Remember, to get proper anti-phasic gait, or better put, to slow the tendency towards spinal protective phasic gait, you need the pelvic and shoulder “girdles” to cooperate. When you get it right, opposite arm and leg will swing together in same pendulum direction, and this will be matched and set up by an antiphasic gait.
One last thing, rushing to the right forefoot will force an early departure off that right limb during gait, which will have to be caught by the left quad to dampen the premature load on the left. They will also likely have a left frontal plane pelvis drift which will also have to be addressed at some point or concurrently. This could set up a cross over gait in some folks, so watch for that as well.
“One thing, affects all things. One change necessitates global change. The more you know, the more you will see (and understand). The more you know, see and understand, the more responsible you will and should feel to get it right and the more global your approach should become. If your head does not spin at times with all the issues that need to be juggled, you are likely not seeing all the issues you should be seeing.” -Dr. Allen (from an upcoming CME course)
Shawn Allen, one of the gait guys.